Indexed in: ESCI, Scopus, PubMed,
PubMed Central, CAS, DOAJ, KCI
PubMed Central, CAS, DOAJ, KCI
FREE article processing charge

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(Suppl); 2023 > Article
-
Case report
Shunt fracture as a sequela of cervical spine manipulation: a case report -
El Kim

-
Journal of Yeungnam Medical Science 2023;40(Suppl):S109-S112.
DOI: https://doi.org/10.12701/jyms.2023.00479
Published online: July 17, 2023
Department of Neurosurgery, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- Corresponding author: El Kim, MD, PhD Department of Neurosurgery, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, 1035 Dalgubeol-daero, Dalseo-gu, Daegu 42601, Korea Tel: +82-53-258-4385 • Fax:+82-53-258-4388 • E-mail: bach1158@dsmc.or.kr
• Received: May 9, 2023 • Revised: June 14, 2023 • Accepted: June 19, 2023
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,123 Views
- 37 Download
Abstract
- Shunt disconnection is an unreported complication of spinal mobilization and manipulation. We present the case of a young adult who underwent cystoperitoneal (CP) shunt placement for an arachnoid cyst at the age of 6 years. The shunt remained functional during a follow-up period of 11 years. The patient was admitted with headache and diplopia that started after cervical manipulation by a chiropractor. Radiography revealed fracture of the distal catheter and resultant enlargement of the temporosylvian cyst. The patient required replacement of the disconnected tubing caudal to the shunt valve. The distal catheter ruptured immediately below the outlet connector of the valve. The symptoms and signs resolved completely after insertion of a new distal tube into the peritoneum. This case report demonstrates that chiropractic manipulation of the neck may be a cause of tubing breakage in patients with CP shunts.
- Spinal manipulation is widely used as an alternative therapy for neck and back pain. This procedure is a passive forced mobilization that can move joint elements beyond their range of motion. Patients typically consider this complementary therapy safe and effective. However, numerous adverse events have been associated with spinal chiropractic treatments, although their reported incidence is low [1].
- Cystoperitoneal (CP) shunting is a viable intervention for symptomatic cerebral arachnoid cysts (ACs) owing to its simplicity and rapid achievement of radiological resolution [2]. Nonetheless, fractures or disconnections are common causes of mechanical dysfunction in shunted patients [3]. Shunt failure associated with chiropractic trauma to the hardware has not been documented previously. This study aimed to illustrate the rare occurrence of a shunt fracture after cervical manipulation in a young adult with a CP shunt for Sylvian AC.
Introduction
- Ethical statements: This study was reviewed and approved by the Institutional Review Board (IRB) of Keimyung University Dongsan Hospital (IRB No: 2023-02-023). Written informed consent was obtained from the patient to participate in the study.
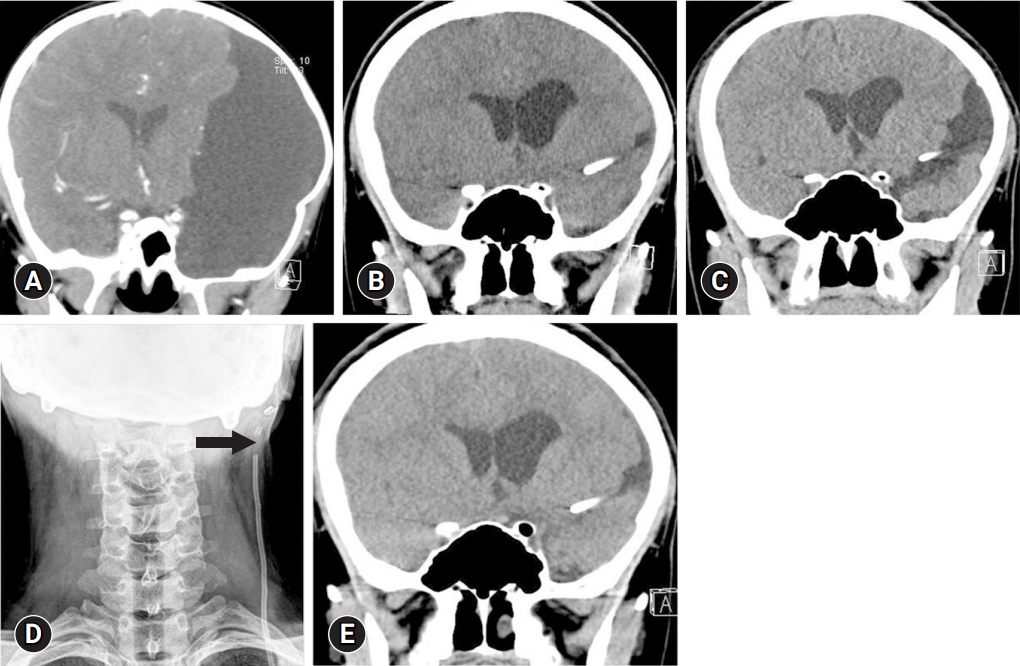
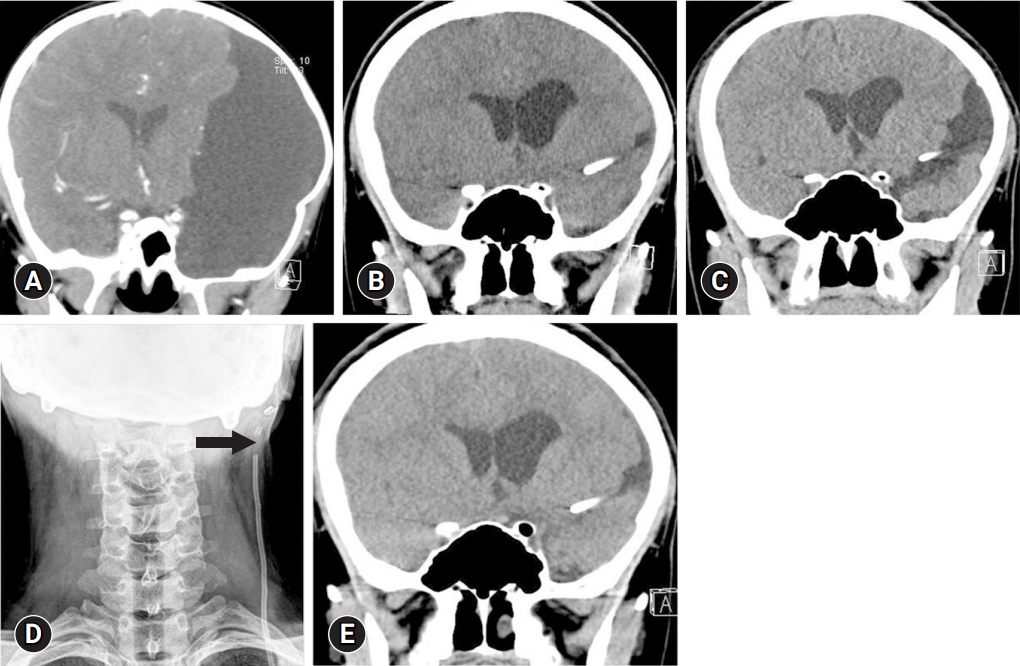
- A 17-year-old male patient complained of progressive headache and double vision with subacute onset. At 6 years of age, the patient underwent CP shunt placement for a large AC in the left Sylvian fissure (Fig. 1A). A Strata system (Medtronic, Goleta, CA, USA) with a programmable pressure valve was placed at the temporal squama. Computed tomography (CT) revealed cyst volume reduction and a return to more normal temporosylvian anatomy (Fig. 1B). The shunt had remained patent prior to the current admission. However, the patient recently visited a chiropractor to relieve cervical discomfort. Manipulation therapy was administered to the implantation site in the occiput and neck for approximately 6 weeks. The patient reported having been subjected to cervical traction and rotational head movements. The last session was performed 1 week before visiting the emergency department.
- The patient had partial palsy of the left lateral rectus. A pumping test of the reservoir yielded good refilling. CT confirmed enlargement of the temporal cyst compared to previous control scans (Fig. 1C). Segmental calcification in the shunt tubing was observed near the collarbone on the radiograph. This clearly revealed a catheter fracture immediately below the outlet connector of the valve (Fig. 1D). The opening pressure was 38 cmH2O during lumbar puncture in the lateral decubitus position. Laboratory investigations of the blood and cerebrospinal fluid failed to reveal any acute abnormalities.
- The patient was immediately transferred to the operating room. The cranial end of the shunt tube was found to be broken and positioned caudal to the valve. A small amount of fluid was observed around the fibrous sheath at the disconnection. The operator identified a 14-mm gap between the two ends of the disconnected catheter. Clear fluid flowed freely from the shunt reservoir. The aged tubing was exteriorized by making short incisions perpendicular to the prior shunt tract. A shunt tunnel was created, and a new peritoneal catheter was inserted. Postoperatively, efficient operation of the shunt system was confirmed by head CT (Fig. 1E). The patient showed symptomatic improvement over the next 15 days.
Case
- Shunt fractures result from calcification, fibrosis, and tethering within tissues, which predispose the catheter to rupture when biomechanical tension is applied [3]. A follow-up study showed that aged implants become fragile within an average of 5 years after the appearance of calcification in pediatric patients [4]. Tubing fractures occur most often in children when their height increases rapidly. During a growth spurt, the distal component is subjected to maximal traction at the connection between the shunt valve and anchoring at the peritoneal wall. In most cases of growth-related strain on the hardware, fractures of the shunt tubing are located just proximal to the clavicle in the neck [5]. Characteristically, however, the drainage tube was broken far from the common location of its disconnection, and shunt calcification was not observed at the fracture site for the current case.
- Common clinical features related to underdrainage due to fractured shunts include headache, vomiting, visual impairment, drowsiness, and gait disturbance [6]. In rare cases, delayed presentation of headache may raise the possibility of shunt dependency syndrome in patients with shunted ACs without tubing fractures [7]. Patients may also present with redness, pain, or fluid over the shunt pathway at the site of the fracture or disconnection [3-5]. Infrequently, the presence of a fibrous sheath enveloping the distal passage explains why the shunt system remains functional even when it is fractured and disconnected [8]. Tubing discontinuation can be considered when there is evidence of anatomical changes in the shunt system, cerebral cysts, or the ventricular system. In addition, the broken shunt no longer functions and can potentially move upward or downward into the extraperitoneal spaces.
- Patients with fractured shunts must undergo reoperation, the timing of which is mainly dictated by their neurological status [3,6]. Surgical revision is performed on an urgent schedule in patients with increased intracranial pressure, as in the present case. In particular, open or endoscopic cyst fenestration could be considered as the first-line option for selected dysfunctional CP shunts when opening the cyst to the basal cisterns is possible. This internal drainage can leave the patient shunt-independent, and it may be followed by external shunting, if indicated [9].
- Cervical manipulations consist of a series of forced and repetitive adjustments involving the combined motions of flexion, extension, rotation, or lateral flexion of a definite vertebral segment [1]. Chiropractic therapy is potentially harmful to patients even when each session is administered by a qualified professional. Despite this, radiological screening of this patient's underlying comorbidities was not performed before spinal manipulation. Sudden thrust or high-velocity, low-amplitude manipulations applied to certain areas of the neck are often considered the cause of untoward reactions to chiropractic mobilization [10]. Although rare, this approach has given rise to complications, such as cervical radiculopathy, stroke, cervical arterial dissection, spinal cord injury, intracranial hypotension, retinal hemorrhage, vertebral fracture, spinal epidural hematoma, and retinal artery occlusion [11,12].
- To raise awareness, a better understanding of manipulation-induced complications is essential for both patients and practitioners. In general, a trained chiropractor tends to manipulate the cervical spine in younger patients more vigorously, thereby increasing the risk of iatrogenic injury to indwelling catheters in the head and neck [1,12]. In our patient, a more aggressive therapy was theorized to cause rotation of the extended neck, resulting in extraordinary stress at the potential tethering between the calcified shunt segment and the valve outlet connector. Biomechanically, this enhanced shearing force was a major contributor to the atypical site of rupture at the cervical portion of the distal drainage [13]. We also have found reports of breakage following the application of strain to the shunt during deformity correction with the aid of halo traction and instrumentation in preadolescents and adolescents with neuromuscular scoliosis [14,15]. It is reasonable to assume that the mechanism of fatigue fracture in these reports was the same as that in our patient, who received neck traction and rotation. Therefore, this case report emphasizes that clinicians should carefully monitor young patients with cerebrospinal fluid shunt systems when they have undergone cervical spine chiropractic therapy or realignment of scoliosis.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
Notes
Fig. 1.Fracture of cystoperitoneal (CP) shunt following cervical chiropractic therapy. (A) An enhanced coronal computed tomography (CT) image shows a large arachnoid cyst with remarkable mass effect. (B) Head CT taken 2 years after the CP shunt reveals disappearance of the Sylvian cyst. (C) Admission CT scan depicts a regrowing cyst and its mass effect on the cerebral cortex. (D) Neck X-ray discloses breakage of the shunt tubing at its cervical portion (arrow). (E) There is complete resolution of the cyst recurrence following the revision shunt surgery.
- 1. Ernst E. Chiropractic: a critical evaluation. J Pain Symptom Manage 2008;35:544–62.ArticlePubMed
- 2. Arai H, Sato K, Wachi A, Okuda O, Takeda N. Arachnoid cysts of the middle cranial fossa: experience with 77 patients who were treated with cystoperitoneal shunting. Neurosurgery 1996;39:1108–13.ArticlePubMed
- 3. Erol FS, Ozturk S, Akgun B, Kaplan M. Ventriculoperitoneal shunt malfunction caused by fractures and disconnections over 10 years of follow-up. Childs Nerv Syst 2017;33:475–81.ArticlePubMedPDF
- 4. Lee L, Low S, Low D, Ng LP, Nolan C, Seow WT. Late pediatric ventriculoperitoneal shunt failures: a Singapore tertiary institution’s experience. Neurosurg Focus 2016;41:E7.Article
- 5. Kural C, Kirik A, Pusat S, Senturk T, Izci Y. Late calcification and rupture: a rare complication of ventriculoperitoneal shunting. Turk Neurosurg 2012;22:779–82.ArticlePubMed
- 6. Yamamoto S, Ohno K, Aoyagi M, Ichinose S, Hirakawa K. Calcific deposits on degraded shunt catheters: long-term follow-up of V-P shunts and late complications in three cases. Childs Nerv Syst 2002;18:19–25.ArticlePubMedPDF
- 7. Kim SK, Cho BK, Chung YN, Kim HS, Wang KC. Shunt dependency in shunted arachnoid cyst: a reason to avoid shunting. Pediatr Neurosurg 2002;37:178–85.ArticlePubMedPDF
- 8. Clyde BL, Albright AL. Evidence for a patent fibrous tract in fractured, outgrown, or disconnected ventriculoperitoneal shunts. Pediatr Neurosurg 1995;23:20–5.ArticlePubMedPDF
- 9. Gong W, Wang XD, Liu YT, Sun Z, Deng YG, Wu SM, et al. Intracranial drainage versus extracranial shunt in the treatment of intracranial arachnoid cysts: a meta-analysis. Childs Nerv Syst 2022;38:1955–63.ArticlePubMedPDF
- 10. Puentedura EJ, March J, Anders J, Perez A, Landers MR, Wallmann HW, et al. Safety of cervical spine manipulation: are adverse events preventable and are manipulations being performed appropriately?: a review of 134 case reports. J Man Manip Ther 2012;20:66–74.ArticlePubMedPMC
- 11. Kranenburg HA, Schmitt MA, Puentedura EJ, Luijckx GJ, van der Schans CP. Adverse events associated with the use of cervical spine manipulation or mobilization and patient characteristics: a systematic review. Musculoskelet Sci Pract 2017;28:32–8.ArticlePubMed
- 12. Albuquerque FC, Hu YC, Dashti SR, Abla AA, Clark JC, Alkire B, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg 2011;115:1197–205.ArticlePubMed
- 13. Langmoen IA, Lundar T, Vatne K, Hovind KH. Occurrence and management of fractured peripheral catheters in CSF shunts. Childs Nerv Syst 1992;8:222–5.ArticlePubMedPDF
- 14. Hoover D, Ganju A, Shaffrey CI, Bartkowski H, Rauzzino MJ. Shunt fracture following correction of spinal deformity. Case illustration. J Neurosurg 2000;92(1 Suppl):122.Article
- 15. Blakeney WG, D’Amato C. Ventriculoperitoneal shunt fracture following application of halo-gravity traction: a case report. J Pediatr Orthop 2015;35:e52–4.ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite


