PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 41(2); 2024 > Article
-
Review article
Patient-physician interaction education in Korea: a systematic review -
Hwan Ho Lee1,*
 , Yu Ra Kim2,*
, Yu Ra Kim2,* , Hye Jin Park3
, Hye Jin Park3
-
Journal of Yeungnam Medical Science 2024;41(2):74-79.
DOI: https://doi.org/10.12701/jyms.2023.01109
Published online: February 5, 2024
1Department of Otolaryngology-Head and Neck Surgery, Kosin University College of Medicine, Busan, Korea
2Department of Medical Education and Humanities, Yeungnam University College of Medicine, Daegu, Korea
3Department of Medical Education, Eulji University School of Medicine, Daejeon, Korea
- Corresponding author: Hye Jin Park, PhD Department of Medical Education, Eulji University School of Medicine, 90 Gyeryong-ro 771beon-gil, Jung-gu, Daejeon 34824, Korea Tel: +82-42-259-1616 • Fax: +82-504-017-5515 • E-mail: parkhj@eulji.ac.kr
- *These authors contributed equally to this work as co-first authors.
© 2024 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,259 Views
- 56 Download
Abstract
- Patient-physician interaction (PPI) is an important area in medical education, but in-depth discussions on the content of the outcome of patient-doctor education are rare. Therefore, in this study, we will systematically analyze the research on PPI education in Korea. In this study, papers searched with keywords related to PPI education from Korea’s academic journal service were targeted according to a systematic literature analysis method. The scope of the study was to include papers published in academic journals that are candidates for Korea Citation Index registration, excluding dissertations, research reports, posters, conference presentations, books, and internet materials. The content included papers targeting medical education and medical school students was set as the range. As a result of the analysis, although communication between PPI has many positive effects in the PPI in medical education at medical schools, obstacles do occur, and various ways to overcome them were suggested. Therefore, although medical interview training between patients and doctors in medical schools is necessary, it was analyzed as being based on overseas research or lacking in specific content. The core of PPI education appears to be medical interviews, and it seems necessary to discuss whether empathy or patient-centered medical care are appropriate as the main principles of PPI education in Korea. Therefore, education on the patient-doctor relationship is an important element in medical humanities and medical humanities education, and it is expected that research and education on this will progress more actively.
- Although medicine has developed remarkably with scientific medicine, problems such as the dehumanization of medical care and alienation of patients from diseases have arisen, and modern medical education emphasizes medical humanities as one of the solutions to these problems [1]. The core of medical humanities begins with valuing human beings in the medical field. Physician treatment of patients is one of the most important tasks in the medical field, and the accompanying doctor-patient relationship is one of the important elements of medical education.
- The importance of the patient-physician interaction (PPI) in the medical field cannot be overemphasized [2]. The Hippocratic Oath, which contains Hippocratic thought, is still recited at the White Coat Ceremony [3], a welcome party for freshmen, or a graduation ceremony [4]. The core of the Hippocratic Oath is a declaration by physicians about the relationship between patient and physician. In this way, the PPI is at the center of discussions on what kind of physicians to train in the era of advanced medicine in the 21st century [2].
- As Korea became the first Asian country to introduce a practical test (six medical questions, six written questions) in the national medical examination in 2009, all medical questions included the same question about the PPI, and each school became interested in education on this [5]. Furthermore, from 2022, as the practical tests of the national medical examination are all changed to medical questions (10 items), the PPI is more emphasized in medical education.
- However, PPI education is sometimes used in combination with the results of the same or oriented direction as the core keywords in medical humanities such as medical interview, patient-centeredness, and patient safety. There are studies on PPI education in medical interviews, patient-physician orientation [2], and relationships with empathy [6], and it was difficult to confirm in-depth discussions on the outcomes and contents of PPI education. Therefore, this study aims to systematically analyze research on PPI education in Korea.
Introduction
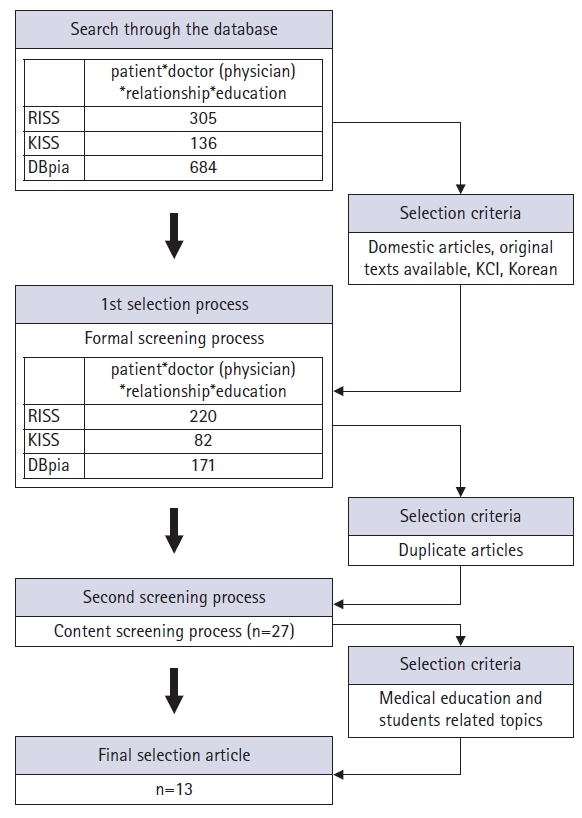
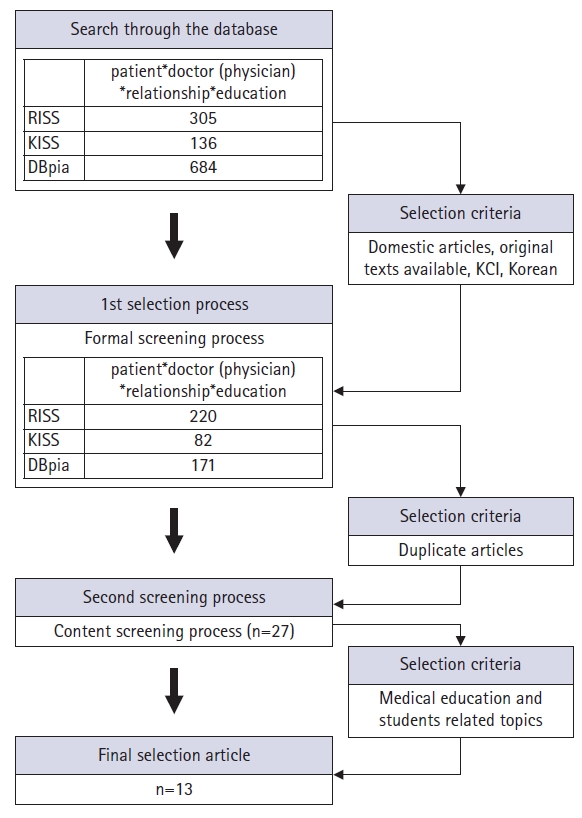
- From June 15 to 22, 2023, research trends in papers searched for keywords related to PPI education were identified in the thesis base. The selection criteria for papers in this study are as follows.
- First, it was limited to Korea, patients, physicians, relationships, and education, and the time of presentation was not limited. Second, papers published in academic journals listed (candidate) or higher in the Korea Citation Index were targeted, and dissertations, research reports, posters, presentations at academic conferences, books, and internet materials were excluded. Third, it was limited to papers whose original texts could be confirmed. Fourth, this study was limited to papers targeting medical education and medical students. Finally, the scope of the database to be searched was limited to RISS (Research Information Sharing Service, https://www.riss.kr/), KISS (Korean studies Information Service System, https://kiss.kstudy.com/), and DBpia (https://www.dbpia.co.kr/). Search keywords were designated as patient & physician & relationship & education.
- Two medical education experts participated in this study and discussed the collection and selection of papers, derivation of analysis standards, and coding and analysis results through online and offline meetings. By the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [7], the bias and subjectivity of the study were eliminated, and research issues were clarified with the research trend of PPI education in Korea. A comprehensive conclusion of the study was drawn by proceeding in the order of paper search, paper selection, analysis result, and discussion [8].
- As a result of searching the paper database according to the scope and criteria of papers, 684 papers were searched, and 220 papers were selected through the primary screening process. Twenty-seven papers were selected through the second screening process, and 13 papers were derived through the final screening process (Fig. 1).
Design
- 1. The importance of communication between physician and patient
- Appropriate communication between the patient and the physician is important because it provides a pathway to accurate diagnosis and appropriate treatment based on mutual trust [5]. Appropriate communication between physician and patient showed high patient satisfaction, and the rate of lawsuits due to medical errors tended to be low [2,5,9]. Physician communication is known to act as a major factor in satisfaction and compliance with treatment and to have a positive effect on treatment results and health improvement [5,10,11].
- Appropriate communication between physician and patient can serve not only as a treatment effect but also as a major strategy for medical marketing in the increasingly fierce market competition [12]. Not only medical knowledge and skills but also patient-centered communication competencies and cultures directly influence the evaluation of hospitals and physicians [12].
- 2. Obstacles to medical interviews between physician and patient
- The form of a meeting between a physician and a patient is a meeting between a warm heart (emotion) and a cool head (logic) [13]. Communication between physician and patient is a social communication situation that requires trust and accuracy, and ambiguity or misunderstandings caused by communication problems can lead to misdiagnosis [13]. Through communication between the physician and the patient, it is possible to establish a relationship, evaluate the patient’s problem, and treat it [14].
- Problems identified by analyzing the patient-physician encounter included lack of communication, lack of attention to the patient’s other concerns, unilateral signaling of the end of the encounter by the physician, lack of education about the patient’s disease, lack of communication about the treatment plan, and lack of motivation for treatment [14].
- The following four factors have been reported as obstacles to proper medical interviews [13,14]. First, the structural problems of the medical care system, such as the average interview time per patient, the desk structure of the office, and the patient waiting area, are environments that may impede nonverbal communication. Second, physicians’ communication skills, such as abusing specialized medical terms that patients do not understand, overloading patients with information, using ambiguous language, not empathizing with patients’ feelings, not responding to patients’ questions, and unilaterally terminating appointments. Third, there was an issue of awareness of the rights of the physician, which required consideration of the patient’s right to be fully informed of their illness. Finally, while physicians tended to communicate from a problem-solving perspective, patients reported that they wanted to communicate from a relationship-building perspective, not only to solve problems but also to understand their situation and feelings.
- 3. Ways to overcome obstacles to medical interviews between physician and patient
- Alternatives to overcome obstacles to medical interviews are as follows [13]. Although medical knowledge should be based on rational practice, physicians need to develop and practice patient-centered emotional communication techniques to collect sufficient information from patients in the course of conversation. In addition, physicians need the willingness and assistance to practice a symmetrical relationship in which they view patients as partners on a team in the process of treating disease, and they need to be good listeners and recognize that listening is a communication skill that requires practice. Physicians need to use patient-centered vocabulary about medical history taking, and physicians need to acquire and practice verbal and nonverbal feedback techniques to collect richer and more accurate information from patients.
- 4. Necessity of medical interview education between physician and patient
- Physicians’ communication skills do not improve by themselves [12]. Physicians who have learned communication skills have a strong will to communicate with patients, it becomes easier to empathize with patients, and this leads to confidence in communication with patients [12].
- 5. Overview of medical interview training between physician and patient
- Recognizing the need for medical interview education between physician and patient, domestic medical schools are including education related to medical interviews in their curricula. However, such as Table 1 [5,15,16], related subjects or programs are not specific [12]. Lack of time to study medical knowledge, professionalism of professors, teaching methods, and lecture contents fall short of expectations or are evaluated as too theory-centered [17]. Most of the guidelines for patient-physician medical interviews refer to foreign studies (Table 2) [18-22].
- 6. Effects of medical interview education between physician and patient
- Students who took the medical interview education were better at taking the history (receiving information related to the disease) than those who did not and were more proficient at practicing the medical interview [16]. There was a positive correlation between the student’s communication ability immediately after the medical interview class and the difference in the ability to form a PPI in the clinical performance evaluation measured after a certain period [23].
- Although there are no complete guidelines or principles for medical interviews, since not all medical interview education is effective, the effectiveness can be expected only when appropriate subjects are provided [16].
- 7. Patient-physician interaction based on empathy
- A physician’s empathy plays an important role in forming a PPI, has a positive effect on patient treatment, and improves the quality of medical care [6]. A physician’s empathy ability perceived by a patient is related to patient satisfaction and patient acceptance [24]. The act of communication in which the physician empathizes with the patient and relates emotionally is an important factor in forming trust [25].
- 8. Patient-physician interaction based on patient-centered medical care
- Medical development of science in the 20th century has contributed greatly to human life and health, but on the other hand, medicine based on the biological medicine model has been criticized for making the relationship between patients and physicians too disease-centered [2]. As the need for the patient’s role in the treatment process has recently increased, the importance of patient-centered medical care, which includes the guarantee of patient autonomy and the right to self-determination, is increasing. Although the concept of patient-centered medical care is ambiguous [26], McWhinney (1989) [27] defined the patient-centered approach as ‘entering the patient’s world, to see the illness through the patient’s eyes’ [2]. Patient-centered care consists of medical service, communication, and PPI. It was argued that the most important thing in patient-centered medical care is the PPI because the patient-centered PPI increases smooth communication, and patient satisfaction, and strengthens the physician-patient cooperative relationship as the patient participates in the treatment process [2]. It was argued that communication skills, professionalism, and humanities and social studies education are necessary to establish a patient-centered PPI [2].
Results
- The purpose of this study was to analyze research on PPI education in Korea. As a result, the keyword in PPI education was a medical interview. The importance of the PPI, especially communication and patient interviews, began with Hippocrates oath in ancient times, when human medicine began, and has continued to the present, and its importance has been emphasized more recently. Accordingly, medical schools for training physicians are striving for related education, and among them, medical interviews between physicians and patients have been analyzed as one of the core educational contents in PPI education.
- A medical interview is a kind of communication channel for the patient and physician to share the common goal of treatment, not only helping diagnosis and treatment but also related to patient satisfaction. However, since the medical interview is a social communication situation, it is necessary to convey the knowledge about the disease cognitively as well as emotionally and psychologically, and it was confirmed that various obstacles can occur in this process. As a way to overcome these obstacles, the need for medical interview education has emerged, and the effectiveness of medical interviews has been proven through research. Medical schools in Korea are implementing medical interview education, but the instructional design is evaluated as insufficient or too theoretical, and it is difficult to confirm medical interview guidelines based on the medical situation in Korea. It was confirmed that research on the words empathy and patient-centered medical care was conducted in PPI education.
- PPI education in Korea is mainly carried out through medical interviews, but systematic discussions about the results of medical interview education in Korea, educational contents, educational methods, and evaluation methods do not seem to be actively conducted. In addition, it was confirmed that a series of guideline development studies including the principles of medical interviews reflecting the Korean medical field were necessary. As PPI education is mainly conducted through medical interviews, it is necessary to clarify and educate the relationship, such as whether medical interview education is a means to establish a PPI or whether the PPI is a medical interview. Although the main direction of medical interviews is converging on empathy and patient-centered care, it seems necessary to discuss whether empathy or patient-centered care is appropriate as the main principle in patient-physician relationship education in Korea. Therefore, education on the PPI is an important element in medical humanities and medical humanities education, and it is expected that research and education on this will progress more actively.
Conclusion
-
Conflicts of interest
No potential conflict of interest relevant to this article are reported.
-
Funding
None.
-
Author contributions
Conceptualization: all authors; Data curation, Formal analysis: YRK, HJP; Validation: HHL; Methodology: HHL, HJP; Software, Supervision: HJP; Writing-original draft: YRK, HJP; Writing-review & editing: YRK, HJP.
Article information
| Contents | Note | |
|---|---|---|
| Accomplishment | • Cultivation of empathic communication skills [5] | • Physician job analysis [5] |
| • Cultivation of communication skills to cope with special clinical situations [5] | ||
| Contents | • Basic concepts: general theory of communication, what is communication?, basic concepts of medical communication, medical interview basics, medical communication basics, understanding of medical communication [15] | • United Kingdom: communication on different media (telephone, computer, etc.) [5] |
| • Fundamental skills (interview, questioning, listening, clarification, reflection, silence, empathy, contact, etc.) [15] | ||
| • Relationship-building technique: amicable bond, formation of quasi-verbal and nonverbal communication [15] | ||
| • Understanding the patient: understanding the patient, cultural diversity of the patient, illness, and self-understanding as a communicator [15] | ||
| • Dealing with difficult patients (uncooperative, hostile, suspicious, anxious, dependent, demanding, deaf, pediatric, mentally ill) [5,15,16] | ||
| • Patient education and end of interview: explanatory conversation, counseling and education, information provision technology (education), information sharing technique [15] | ||
| • Interviews by age: including child-adolescent interviews, family interviews, and older adults [15] | ||
| • Delivering bad news (notification of intractable diseases, etc.) [5,16] | ||
| • Medical ethics (legal issues, death with dignity, etc.) [5] | ||
| • Behavior change counseling: patient coaching, motivational interview [15] | ||
| • Others (history of sexual problems, communication with patients from different cultures, mistakes, complaints, lawsuits, etc.) [15,16] | ||
| • Admitting mistakes: error disclosure, transferring mistakes, ignorance disclosure [15] | ||
| • Team communication: asking colleagues for advice, how to report cases [15] | ||
| Methods | • Lecture, discussion, case analysis, demonstration, interview process observation, role play, video analysis, practice using standardized patients [5] | • Japan: with standard patient guidelines [5] |
| SEGUE (2001) [19] | Kalamazoo Consensus (2001) [20] | Calgary-Cambridge Guides (2003) [21] | Macy guideline (2004) [22] |
|---|---|---|---|
| 1. Set the stage | 1. Build a relationship | 1. Initiate session | 1. Allow patient to express self |
| 2. Elicit information | 2. Open the discussion | 2. Gather information | 2. Be attentive and empathic nonverbally |
| 3. Give information | 3. Gather information | 3. Physical examination | 3. Use appropriate language |
| 4. Understand the patient’s perspective | 4. Understand the patient’s perspective | 4. Explanation planning | 4. Communicate nonjudgmental, respectful, and supportive attitude |
| 5. End the encounter | 5. Share information | 5. Closing the session | 5. Accurately recognize emotions and feelings |
| 6. Reach agreement on problems and plans | 6. Use PEARLS statements (Partnership, Empathy, Apology, Respect, Legitimization, Support) to respond to emotion instead of redirecting or pursuing clinical detail | ||
| 7. Provide closure | 7. Be organized and logical | ||
| 8. Manage time effectively in the interview |
- 1. Kwon SO. Conception of medical humanities and it’s role in medical education. Korean J Med Educ 2005;17:217–23.Article
- 2. Park J. Medical students’ attitudes toward the patient-doctor relationship. Korean J Med Educ 2007;19:215–23.Article
- 3. Association of American Medical Colleges (AAMC). Medical student perspective: the white coat ceremony [Internet]. Washington, DC: AAMC; 2020 [cited 2023 Nov 8]. https://students-residents.aamc.org/aspiring-docs-fact-sheets-what-medical-school/medical-student-perspective-white-coat-ceremony.
- 4. Jeong JH. Good Neighbor: Park Jong-hyung, director of Seoul Oriental Medicine Hospital–lowering the threshold of hospitals and opening up open medicine. Saegajeong 1995;(463):46–9.
- 5. Ahn JH. Patient-physician communication in medical education. Health Commun 2010;5:128–33.
- 6. Chun MY, Yoo SH, Park HK. Medical students’ empathy and its effect on the physicianpatient relationship. Korean J Med Educ 2015;27:283–90.ArticlePubMedPMC
- 7. Kim SY, Park JE, Seo HJ, Seo HS, Son HJ, Shin CM, et al. NECA's guidance for undertaking systematic reviews and meta-analyses for intervention. Seoul: National Evidence-based Healthcare Collaborating Agency; 2011.
- 8. Park HJ, Kim YR. Evaluation research in Korean medical education: a systematic review. J Yeungnam Med Sci 2023;40:233–40.ArticlePubMedPMC
- 9. Weinberger M, Greene JY, Mamlin JJ. The impact of clinical encounter events on patient and physician satisfaction. Soc Sci Med E 1981;15:239–44.ArticlePubMed
- 10. Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns 2006;62:347–54.ArticlePubMedPMC
- 11. Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152:1423–33.PubMedPMC
- 12. Lee IW, Kim CS, Lee HS, Lee WS. A content analysis on a form and manner in medical communication subject: focused on the medical schools in Korea. Commun Theor 2015;11:104–41.
- 13. Lee DW. A conversational analysis of ‘doctor-patient’ communication: in search of the interpersonal communication problems and solutions. Korean J Journal Commun Stud 2000;45:232–65.
- 14. Jeon EJ. The characteristics of medical interview and its obstacle. J Speech Commun 2008;13:39–72.
- 15. Kim DH, Roh HR, Shin JS, Park HK, Park EH, Sung NJ, et al. Setting the range of textbook of communication in healthcare by modified Delphi method. Health Commun 2011;6:7–12.Article
- 16. Lloyd M, Bor R. Communication skills for medicine. Kim S, Park JH, Heo YR, translators. Seoul: Academypress; 2008.
- 17. Lee YM. Challenges in communication skills education in medicine: based on personal experience and reflection. Korean J Med Educ 2012;24:65–8.ArticlePubMedPMC
- 18. Kim DH, Yoon HJ, Lee MJ, Ahn JY, Lee SJ, Suh YS. Comparison of patient-physician interaction (PPI) evaluation between different grade medical students. Korean J Med Educ 2010;22:169–76.ArticlePubMed
- 19. Makoul G. The SEGUE Framework for teaching and assessing communication skills. Patient Educ Couns 2001;45:23–34.ArticlePubMed
- 20. Makoul G. Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med 2001;76:390–3.ArticlePubMed
- 21. Kurtz S, Silverman J, Benson J, Draper J. Marrying content and process in clinical method teaching: enhancing the Calgary-Cambridge guides. Acad Med 2003;78:802–9.ArticlePubMed
- 22. Kalet A, Pugnaire MP, Cole-Kelly K, Janicik R, Ferrara E, Schwartz MD, et al. Teaching communication in clinical clerkships: models from the macy initiative in health communications. Acad Med 2004;79:511–20.ArticlePubMed
- 23. Lee YM, Kim BS. Association between student performance in a medical communication skills course and patient-physician interaction scores on a clinical performance examination. Korean J Med Educ 2008;20:313–20.Article
- 24. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof 2004;27:237–51.ArticlePubMedPDF
- 25. Kim MJ. An exploratory study on the meaning of ‘the patient trusts the doctor’. J Korea Contents Assoc 2017;17:415–23.
- 26. Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns 2002;48:51–61.ArticlePubMed
- 27. McWhinney I. The need for a transformed clinical method. In: Stewart M, Roter D, editors. Communicating with medical patients. Newbury Park, CA: Sage Publications; 1989. p. 25–40.
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite