PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 39(4); 2022 > Article
-
Original article
Effects of early clinical and basic laboratory exposure program on premedical students: a questionnaire survey -
Kyu Hyang Cho1
 , Hyun Sook Ko2
, Hyun Sook Ko2 , Kyung Hee Lee3
, Kyung Hee Lee3 , Tae-Yoon Hwang4
, Tae-Yoon Hwang4 , Keun-Mi Lee5
, Keun-Mi Lee5 , Sae Yoon Kim6
, Sae Yoon Kim6 , Min Cheol Chang7
, Min Cheol Chang7
-
Journal of Yeungnam Medical Science 2022;39(4):309-313.
DOI: https://doi.org/10.12701/jyms.2022.00318
Published online: July 20, 2022
1Division of Nephrology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
2Center for Medical Education, Yeungnam University College of Medicine, Daegu, Korea
3Department of Hematology-Oncology, Yeungnam University College of Medicine, Daegu, Korea
4Department of Preventive Medicine and Public Health, Yeungnam University College of Medicine, Daegu, Korea
5Department of Family Medicine, Yeungnam University College of Medicine, Daegu, Korea
6Department of Pediatrics, Yeungnam University College of Medicine, Daegu, Korea
7Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, Daegu, Korea
- Corresponding author: Min Cheol Chang, MD Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, 170 Hyeonchung-ro, Nam-gu, Daegu 42415, Korea Tel: +82-53-620-4682 • Fax: +0504-231-8694 • E-mail: wheel633@gmail.com
Copyright © 2022 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,768 Views
- 57 Download
Abstract
-
Background
- Because premed students do not take courses related to medicine during their first 2 years, they cannot establish their identity as students at medical schools, making it difficult for them to set goals as future doctors. We conducted an early clinical and basic laboratory exposure program for premed students and studied the effects of the program and student satisfaction levels.
-
Methods
- We performed an early clinical and basic laboratory exposure program for premed students for 2 days and evaluated the effects of the program and student satisfaction with it. The program consisted of two types: type 1, where two to four students formed a group, which was assigned to a particular department to participate and make observations during ward rounds, outpatient clinics, examinations, procedures, and surgeries (in the case of basic laboratory work, the students partook in experimental observations); and type 2, where one student followed a medical school professor to observe the professor’s day. After the program ended, an online survey was conducted to investigate the effects on students, their thoughts, and satisfaction levels.
-
Results
- In total, 114 students (91.2%) responded to the survey. Approximately 94% of them were satisfied with the program. They found that the program would be useful for deciding on future career paths, gaining knowledge about a department of interest, studying for a medical program after premedical studies, and befriending residents and professors in certain departments.
-
Conclusion
- Early clinical and basic laboratory exposure programs are recommended for premedical students.
- In South Korea, most medical schools require 6 years to complete. The enrolled students are premedical students during the first 2 years, when they take various liberal arts, English, and basic science courses. In the following 4 years, they become medical students and focus on major courses related to medicine. First-year medical students take courses in basic medical science such as anatomy, histology, physiology, biochemistry, pharmacology, immunology, and microbiology. Second-year students take clinical courses related to practical medicine such as internal medicine, surgery, pediatrics, obstetrics and gynecology, and psychiatry. Finally, third- and fourth-year students participate in clerkships in which they engage in practical training within clinical sites at each hospital department.
- The abovementioned system requires students to expend much time and effort into medical studies during their time at medical school, drawing attention away from premedical studies [1]. Furthermore, since premedical students do not take courses related to medicine during their first 2 years, they cannot establish their identity as students at medical schools, making it difficult for them to set goals as future doctors. Furthermore, many premedical students experience difficulty in understanding the relevancy of their courses to their future occupations as doctors.
- Numerous medical schools worldwide offer early clinical exposure programs in which students are taught how the courses they take before practical training at hospitals are related to the actual role of medical doctors [2-5]. These programs encompass a variety of forms, including strictly observational and limited hands-on exposure, and they are known not only to expand the understanding of courses before practical training but also to raise student interest in the profession itself [2-5]. However, little is known about the satisfaction levels of students who participate in early clinical and basic laboratory exposure programs.
- We conducted an early clinical and basic laboratory exposure program for first- and second-year premedical students and studied the effects of the program and student satisfaction levels with it.
Introduction
- Ethical statements: This study was approved by the Institutional Review Board (IRB) of Yeungnam University Hospital (IRB No: 2021-09-054). The informed consent was waived due to the retrospective nature of the study.
- 1. Program implementation
- The program was implemented between August 24 and 25, 2021, for second-year premedical students and between August 26 and 27, 2021, for first-year premedical students. Departments and students wishing to participate in the program were recruited, and participation was voluntary. Students were assigned departments according to their first, second, and third preferences and on a first-come-first-serve basis for popular choices (Table 1).
- Before the program, students were taught a 1-hour course on infection prevention, hospital facilities, and precautions to implement when entering operating rooms. The program consisted of two types. For the type 1 program, two to four students formed a group that was assigned to a particular department to participate in and make observations during ward rounds, outpatient clinics, examinations, procedures, and surgeries (in the case of basic laboratory work, the students partook in experimental observations). For the type 2 program, one student followed a medical school professor to observe the professor’s daily routine. The program began at 8 ᴀᴍ and ended at 5:30 ᴘᴍ (Table 2).
- 2. Survey
- After the program ended, a survey was conducted anonymously online for 1 week (Aug 26 to Sep 2, 2021) to investigate students’ thoughts and satisfaction levels, and effects of the program (Table 3).
- General characteristics, including sex, year, department, and program type, were surveyed. Students were asked to provide a single answer to multiple-choice questions on their expectations of the program, whether they researched the relevant department before entering the program, their level of satisfaction, the challenges they faced, and what they gained through the program. They were also asked to write a short answer, suggesting potential improvements to the program. The survey results were retrospectively analyzed.
Methods
- Twenty-three departments participated in the program (20 departments participated in the type 1 program and 13 professors in 10 departments participated in the type 2 program). Of the 73 second-year and 71 first-year students, 66 (90.4%) and 59 (83.1%) joined the program, respectively. Among the participants, 114 students (male:female, 82:32), 61 second-year (92.4%) and 53 first-year (89.8%) students, responded to the survey. Eighty-eight patients participated in the type 1 program, and 26 patients participated in the type 2 program.
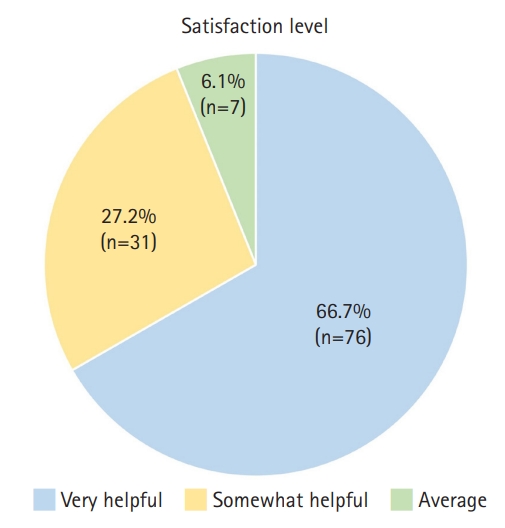
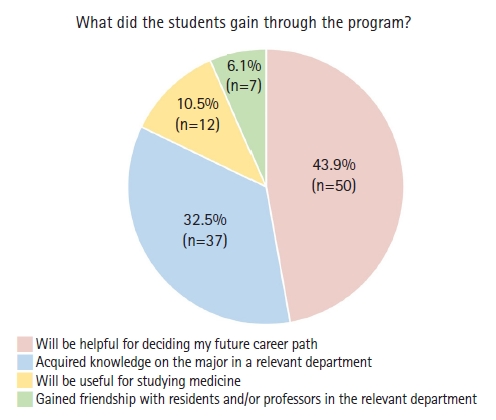
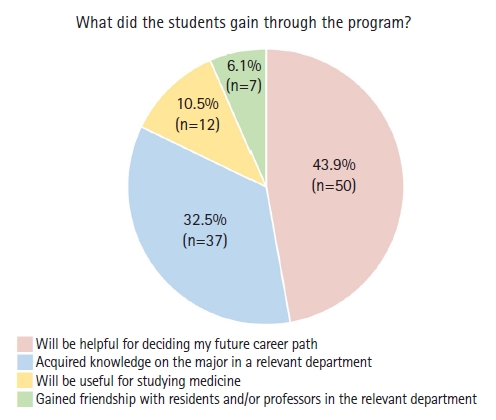
- Regarding expectations of the program, the most common response was “get to know projects undertaken in interested department” from 86 students (75.4%), followed by “befriend the residents and/or professors in relevant department” from 16 students (14.0%). In addition, 51 students (44.7%) did not research relevant departments before participating in the program, 44 students (38.6%) searched the internet for information, and 17 students (14.9%) asked senior class members. Regarding the question on satisfaction level, 76 students (66.7%) found the program very helpful, 31 students (27.2%) thought it was somewhat helpful, and seven students (6.1%) responded that it was average (Fig. 1). No student found the program unhelpful. On the question about challenging aspects of the program, the most common response was “no challenges” from 46 students (40.4%), followed by “lack of basic knowledge” from 39 students (34.2%), and “too much free time made me bored” from 12 students (10.5%). Finally, for the question on what the students gained through the program, 50 students (43.9%) answered “will be helpful for deciding my future career path,” followed by “acquired knowledge on the major in a relevant department” from 37 students (32.5%), “will be useful for studying medicine” from 12 students (10.5%), and “gained friendship with residents and/or professors in the relevant department” from seven students (6.1%) (Fig. 2).
- With respect to the short answer question on potential improvements to the program, some common responses were “would like to have introductory lectures on relevant department before practical training,” “the content of program varied drastically between departments and professors,” “would like to experience more than two departments,” and “would like a program of longer duration.”
Results
- The present study implemented an early clinical and basic laboratory exposure program for premedical students, which received positive feedback and high levels of satisfaction.
- Of the program participants. 94% indicated satisfaction with the program. The students found the program useful for deciding their future career paths, gaining knowledge about a department of interest, studying for a post-premed medical program, and befriending residents and professors in certain departments. The program was deemed helpful for the students’ intent to set goals for themselves as doctors, to improve the academic connection between premedical and medical programs by acquiring medical knowledge in advance, and to establish an identity as medical school students. In particular, during the coronavirus disease 2019 (COVID-19) pandemic that necessitated contactless meetings, the program facilitated bonding between students, residents, and professors [6].
- Of the students who took part in the program, 34% found it challenging due to a lack of basic medical knowledge, while 10% were bored because there was too much free time. Therefore, in future programs, it would be more beneficial for students if participating departments offered offline or online orientations or introductory booklets and organized a tighter schedule. Furthermore, once the program is firmly established, lengthening its duration and allowing students to participate in more than two departments may be considered.
- Previous studies have focused on the effects of early clinical exposure programs, which, according to medical studies, produce a high level of satisfaction and raise student confidence when treating patients [2-5]. However, these studies only investigated medical students who were taking medicine-related courses. We carried out an early exposure program for premedical students who were taking liberal arts and basic science courses and observed positive effects and responses. To the best of our knowledge, this study is the first to implement an early exposure program for premedical students who have not started taking major-related medical courses.
- Considering the 6 years of medical school education, with 2 years in the premedical program and 4 years in the medical program, this study assessed early clinical and basic laboratory exposure programs for first- and second-year premedical students. We observed that over 90% of the participants were satisfied with the program and witnessed various positive effects. To raise the quality of future programs, each department should provide information in advance and work with professors to create a full schedule. Future studies should analyze factors that may have influenced student satisfaction levels and measure satisfaction levels and effects according to department and program type, which this study did not examine. Our study had some limitations. First, the development process of the satisfaction evaluation tool was not clearly described. Second, open-ended questions and interviewers were not included. Third, the sample size was not sufficiently large to clearly demonstrate the satisfaction level for early clinical and basic laboratory exposure programs. Finally, the outcome measurements in our study were relatively simple, and measurements of educational outcomes and changes in the actual performance of participating students are necessary. Further studies addressing these limitations are required in the future.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization: all authors; Methodology: KHC, HSK, MCC; Investigation: all authors; Data curation, Formal analysis, Validation: KHC, MCC; Project administration, Visualization: MCC; Resources: all authors; Supervision: MCC; Writing-original draft: all authors; Writing-review & editing: all authors.
Notes
- 1. Gross JP, Mommaerts CD, Earl D, De Vries RG. Perspective: after a century of criticizing premedical education, are we missing the point? Acad Med 2008;83:516–20.ArticlePubMed
- 2. Başak O, Yaphe J, Spiegel W, Wilm S, Carelli F, Metsemakers JF. Early clinical exposure in medical curricula across Europe: an overview. Eur J Gen Pract 2009;15:4–10.ArticlePubMed
- 3. Chang CC, Huang HC, Lee WS, Chuang CL, Huang LJ, Lu DY, et al. Early clinical exposure improves medical students' recognition of the need for professionalism and interprofessional collaboration. J Chin Med Assoc 2021;84:778–82.ArticlePubMed
- 4. Davis JM, Anderson MC, Stankevitz KA, Manley AR. Providing premedical students with quality clinical and research experience: the Tobacco Science Scholars Program. WMJ 2013;112:195–8.PubMedPMC
- 5. Tang KP, Chen CY, Wu MS, Chen TT, Wu BW, Tsai PF. Correlation between early clinical exposure environment, attitudes toward basic medicine, and medical students’ basic science learning performance. BMC Med Educ 2019;19:183.ArticlePubMedPMCPDF
- 6. Franklin G, Martin C, Ruszaj M, Matin M, Kataria A, Hu J, et al. How the COVID-19 pandemic impacted medical education during the last year of medical school: a class survey. Life (Basel) 2021;11:294.ArticlePubMedPMC
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine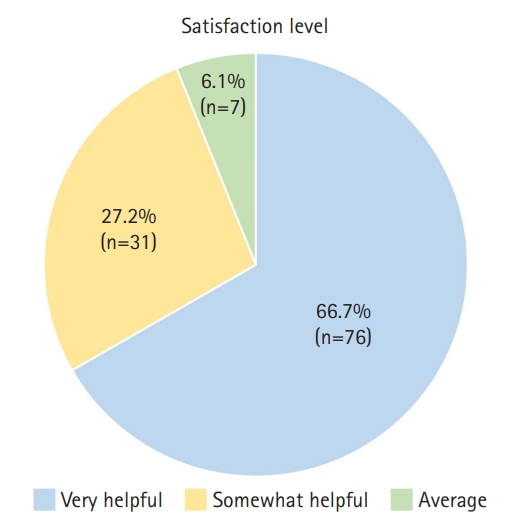
 PubReader
PubReader ePub Link
ePub Link Cite
Cite