PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 38(4); 2021 > Article
-
Case report
Cardiopulmonary bypass preparation is mandatory in cardiac exploration for blunt cardiac injury patients: two case reports -
Shin-Ah Son
 , Joon Yong Cho
, Joon Yong Cho , Gun-Jik Kim
, Gun-Jik Kim , Young Ok Lee
, Young Ok Lee , Hanna Jung
, Hanna Jung , Tak-Hyuk Oh
, Tak-Hyuk Oh
-
Yeungnam University Journal of Medicine 2021;38(4):356-360.
DOI: https://doi.org/10.12701/yujm.2020.00822
Published online: March 3, 2021
Department of Thoracic and Cardiovascular Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- Corresponding author: Tak-Hyuk Oh, MD Department of Thoracic and Cardiovascular Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, 130 Dongdeok-ro, Jung-gu, Daegu 41944, Korea Tel: +82-53-200-5665 Fax: +82-53-426-4765 E-mail: ohhidongii@gmail.com
Copyright © 2021 Yeungnam University College of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 5,313 Views
- 76 Download
- 1 Crossref
Abstract
- Treating cardiac injuries following blunt trauma to the chest requires thorough examination, accurate diagnosis, and therapeutic plan. We present two cases; pulmonary vein rupture and left atrial appendage laceration, both as a result of blunt chest trauma. Through these cases, our team learned the importance of maintaining hemodynamic stability during the examination of injured cardiac structures. And based on the comprehensive cardiac examination, a decision to surgically intervene with median sternotomy via cardiopulmonary bypass was made, saving lives of the patient. This report introduces how such decision was made based on what supporting evidence and the diagnostic process leading to the initiation of surgical intervention. This report may help with decision-making process when confronted by blunt cardiac injury patients who need cardiac exploration.
- Blunt cardiac injury (BCI) following chest trauma is one of the most devastating injuries related to vehicular accidents that cardiac surgeons encounter. About 70% of blunt cardiac injuries occur in the right atrium (RA) and the right ventricle (RV) [1,2]. Although certain injuries may be repairable without cardiopulmonary bypass (CPB), it is difficult to identify the bleeding point preoperatively.
- Here, we report two cases; pulmonary vein (PV) injury and left atrial (LA) appendage rupture as a result of blunt chest trauma. This report conveys the patient’s survival is depending on the maintenance of hemodynamic stability through CPB during the operation.
Introduction
- 1. Case 1
- A 70-year-old man with hypertension was transferred to our center after a traffic accident. He was in drowsy mental state with a Glasgow Coma Scale of 14. The patient was showing symptoms of chest pain and shortness of breath. Respiratory rate of 21 breaths per minute with an oxygen saturation of 97%, a regular pulse of 101 beats per minute, and blood pressure of 101/61 mmHg was recorded at the moment.
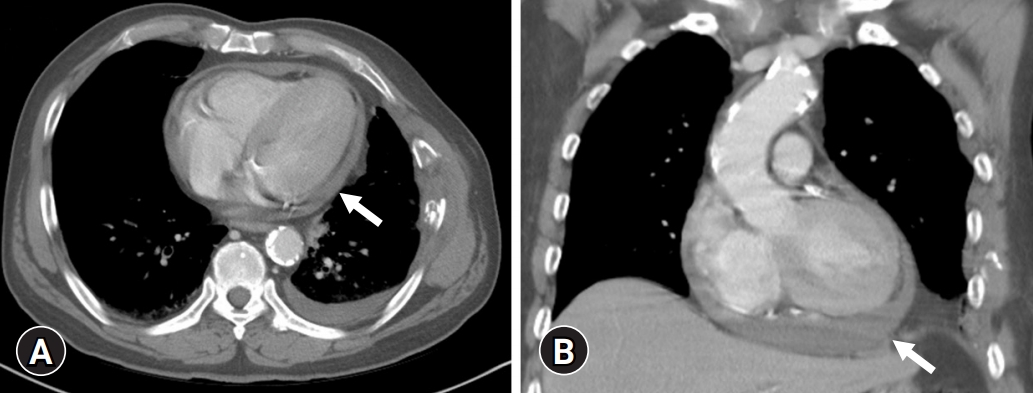
- Computed tomography (CT) after the accident showed a small amount of hemopericardium, but no other vital organ injuries (Fig. 1). Based on these findings, BCI was strongly suspected. Transthoracic echocardiography (TTE) was performed by an experienced cardiologist, which revealed a small pericardial effusion, but the site of injury could not be determined.
- Under general anesthesia, exploratory median sternotomy was performed, and initial vital signs in the operating room were stable. The hematoma in the pericardium and over the RV was removed. In an attempt to visualize the LA and the apex of the left ventricle (LV), sudden massive arterial bleeding occurred. Subsequently, cardiac arrest ensued. While manual compression to the heart was being performed, CPB was established immediately with ascending aortic perfusion and two-staged right atrial venous drainage. CPB circuit priming and cannulation took approximately 20 minutes and open cardiac massage was continued. After achieving cardioplegic arrest, optimal visualization of the operative field was achieved.
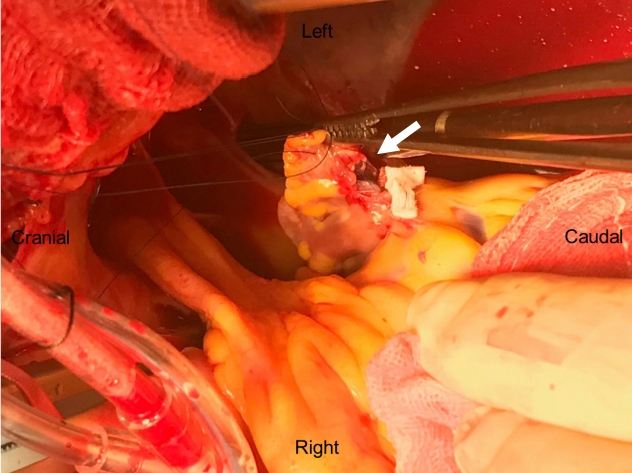
- Careful inspection of the heart revealed a 2-cm laceration of the left upper PV at its junction with the left atrium and the tear was repaired using a Peri-Guard Repair-Patch (Lamed GmbH, Berlin, Germany) and reinforced with 6-0 prolene (Fig. 2). Thorough inspection was performed again under CPB and no further injury was found. However, CPB weaning was difficult due to akinesia of the left anterior descending artery territory. We performed emergency coronary artery bypass surgery and subsequently weaned the patient off CPB. However, he remained in a semi-coma state after cardiac exploration and suffered low cardiac output syndrome (LCOS). Patient’s condition worsened and the patient was pronounced dead on postoperative day (POD) 2. Total aortic cross-clamp and CPB times were 112 and 208 minutes, respectively.
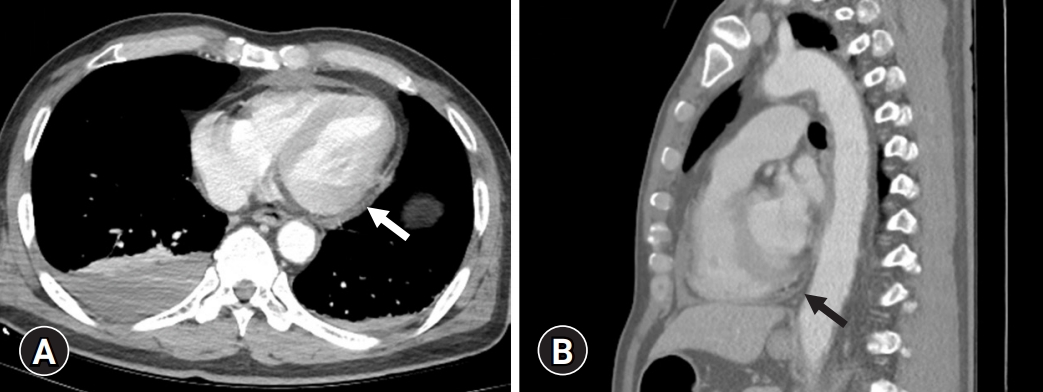
- 2. Case 2
- A 61-year-old man was struck by a motor vehicle while riding his motorcycle and was admitted to our center. The patient’s initial blood pressure and heart rate were 124/72 mmHg and 85 beats per minute, respectively with alert mental status. The CT in the emergency room revealed scanty hemopericardium and right pleural effusion (Fig. 3). Associated injuries were descending colon mesenteric laceration and left distal radius fractures. There were no associated intracranial injuries. RV injury was suspected based on a significant amount of hematoma between the RV and the sternum on CT and decided to perform emergency exploration. However, to avoid unexpected catastrophic situations that may involve hemodynamic instability, CPB was prepared in advance. Through a median sternotomy approach, all the visible blood was removed; however, the active bleeding point was unable to be found. Remaining blood at the base of the heart was visible. In order to thoroughly examine this area, the decision was made to undergo the exploration under CPB assistance. CPB was established by cannulating the ascending aorta and the RA. Venting was performed by placing a cannula into the LA and connecting this to the venous drainage line. After being guaranteed hemodynamic stability, a careful heart inspection was performed by elevating the LV apex. There was bleeding on the LA side coming from a 1.5-cm LA appendage rupture. We repaired the appendage laceration using 4-0 polypropylene suture with polytetrafluoroethylene felt pledget reinforcement, carefully avoiding the left circumflex artery (Fig. 4). No intraoperative event occurred on weaning off bypass. After routine closure, exploratory laparotomy was performed. Aortic cross-clamp and CPB times were 38 and 60 minutes, respectively. The postoperative course was uneventful, and the patient was discharged on the POD 16 after radius fixation operation.
Cases
- BCI due to chest trauma is a fatal condition. Blunt chest trauma occurs up to 50% of all fatal motor accidents and it is known as the primary cause of death in 12% to 25% of such accidents [3]. In a recent report, BCI was seen in 0.045% of blunt trauma patients, with a mortality rate of 89% [1]. One autopsy study of 1,597 fatalities from blunt trauma identified cardiac injuries in 190 individuals (11.9%) [4]. Most BCIs occur due to motor vehicle crashes (approximately 50%), followed by pedestrians being struck by vehicles (35%) and motorcycle crashes (9%), while the remainders are mostly secondary to falls from a significant height [4,5].
- Owing to its anterior location, the RV is the most commonly injured chamber in 40% of BCI patients. The RA and LV follow closely with 30% to 33% of all injuries, PV and LA tears occur in about 1% [2,5]. The mechanism of injury to the venous-atrial confluence, such as the PV is believed to be due to rapid deceleration that allows relatively mobile ventricles to move forward or laterally while the tethered posterior veins do stay stationary [2,4,6,7].
- Therefore, CT scan is a useful tool in initial evaluation of BCI patients. Patients diagnosed with BCI should undergo more advanced imaging such as TTE or transesophageal echocardiography to exclude significant cardiac structural injury. However, these modalities are unable to clearly identify the exact cardiac injury site.
- There have been a number of reports on PV and LA rupture. These reported cases had stable hemodynamics after arrival at the hospital, because the LA and PV circulation is known to be low pressure, low impedance system [3,6,8-11]. Also, isolated injury to these sites as a result of a massive hemothorax is extremely rare [11]. Therefore, it is too dangerous to explore without obtaining hemodynamic stability via CPB. It is difficult to identify the bleeding point preoperatively and the authors in previous reports referred to the advantage of using CPB in these cases [6,8-10,12]. When number and location of bleeding points are uncertain, median sternotomy is beneficial as it permits an easy approach to both sides of the heart as well as easy access to CPB [13-15]. Full examination and repair of the heart and great vessels are easier with CPB because of the bloodless field, decompressed heart, and reduced risk of hemodynamic instability due to sudden blood loss [8]. However, the presence of intracranial bleeding, which is aggravated by complete heparinization, limits the use of CPB [6].
- In the second case, hemoperitoneum was present, however, heparinization did not have a significant effect on bleeding. Therefore, we believe that a short duration of CPB does not increase the risk of bleeding without an existing intracranial bleed.
- In the first case, there was not much hemopericardium and vital signs were stable after arrival, minor RV tearing behind the sternum was suspected. However, the moment the heart was lifted to examine the base, excessive bleeding and cardiac arrest occurred. Although the patient’s femoral vessels were prepared for CPB for such an unexpected situation, it took a considerable amount of time to prime the CPB circuit and to carry out the cannulation.
- In the second case, CPB was performed under the suspicion that the heart base could bleed out and successfully identified cardiac structures without compromising hemodynamics. This report can be used to determine the patient's prognosis which may be different depending on whether or not stable hemodynamics is obtained upon identifying cardiac structures.
- In our trauma center, there have been several cases that underwent cardiac exploration for suspicious BCI after blunt chest trauma (Table 1). Between January 2010 and August 2019, 15 patients underwent cardiac exploration at Kyungpook National University Hospital. Most of these are RA and RV injuries, and CPB was used in seven cases, for which hemodynamic stability was obtained while the cardiac injury was repaired. In three cases, patients had a small hemopericardium and stable vital signs upon arrival, but catastrophic hemorrhage occurred during full cardiac examination, resulting in hurried CPB access. Among them, two patients died from LCOS. In our experience, about 50% of blunt cardiac injuries might be reparable without CPB, but it is difficult to identify the bleeding point preoperatively. Based on this report, the resultant excessive bleeding in the process of examining the full cardiac structure may be managed successfully in hemodynamically stable patients. Therefore, we determined that it is risky to perform cardiac exploration without CPB.
- In conclusion, BCI cases require careful evaluation of the initial CT or TTE and a therapeutic plan that prevents a devastating injury that could result in death. To treat this potentially lethal injury successfully, it is important to maintain hemodynamic stability while inspecting injured cardiac structures, and CPB through a median sternotomy can be a crucial role in saving the patients’ lives. This case report may help with decision making when confronting BCI patients who are in need of cardiac exploration.
Discussion
-
Ethical statements
This study was approved by the Institutional Review Board (IRB) of the Kyungpook National University Hospital (IRB No: KNUH 2020-11-025-001). Written informed consent was obtained from the patient for publication of this case report and accompanying images.
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Author contributions
Conceptualization: SAS, THO; Methodology: JYC, GJK, YOL; Writing-original draft: SAS, HJ; Writing-review & editing: SAS, HJ, THO.
Notes

| Sex/age (yr) | Cause | Amount of hemopericardium | Approach | Injury site | Cardiac arrest in OR | Use of CPB | Outcome |
|---|---|---|---|---|---|---|---|
| Male/46 | Car accident | Small | Median sternotomy conversion in thoracotomy | LA | Yes | Yes | Death |
| Male/55 | Car accident | Small | Thoracotomy | RV | No | No | Discharge |
| Female/41 | Car accident | Small–moderate | Median sternotomy | RA | No | No | Discharge |
| Male/26 | Motorcycle accident | Small | Median sternotomy | Not found | No | No | Discharge |
| Male/56 | Motorcycle accident | Small | Median sternotomy | RV | No | No | Discharge |
| Male/70a) | Car accident | Small | Median sternotomy | PV | Yes | Yes | Death |
| Male/73 | Car accident | Moderate | Median sternotomy | IVC | Yes | Yes | Discharge |
| Male/61b) | Motorcycle accident | Small | Median sternotomy | LA appendage | No | Yes | Discharge |
| Male/50 | Motorcycle accident | Large | Median sternotomy | RV | No | Yes | Discharge |
| Male/63 | Car accident | Small | Thoracotomy | RA | No | No | Discharge |
| Male/57 | Car accident | Small | Median sternotomy | RA, IVC | No | Yes | Discharge |
| Female/44 | Car accident | Moderate | Median sternotomy | IVC | No | Yes | Discharge |
| Male/49 | Fall down | Moderate | Thoracotomy | LV | No | No | Discharge |
| Female/83 | Fall down | Large | Median sternotomy | RV | No | No | Discharge |
| Female/64 | Animal attack | Small | Thoracotomy | RV | No | No | Discharge |
- 1. Teixeira PG, Inaba K, Oncel D, DuBose J, Chan L, Rhee P, et al. Blunt cardiac rupture: a 5-year NTDB analysis. J Trauma 2009;67:788–91.ArticlePubMed
- 2. Turk EE, Tsang YW, Champaneri A, Pueschel K, Byard RW. Cardiac injuries in car occupants in fatal motor vehicle collisions: an autopsy-based study. J Forensic Leg Med 2010;17:339–43.ArticlePubMed
- 3. Hawkins ML, Carraway RP, Ross SE, Johnson RC, Tyndal EC, Laws HL. Pulmonary artery disruption from blunt thoracic trauma. Am Surg 1988;54:148–52.PubMed
- 4. Turan AA, Karayel FA, Akyildiz E, Pakis I, Uzun I, Gurpinar K, et al. Cardiac injuries caused by blunt trauma: an autopsy based assessment of the injury pattern. J Forensic Sci 2010;55:82–4.ArticlePubMed
- 5. Teixeira PG, Inaba K, Barmparas G, Georgiou C, Toms C, Noguchi TT, et al. Blunt thoracic aortic injuries: an autopsy study. J Trauma 2011;70:197–202.ArticlePubMed
- 6. Ouda A, Kappert U, Ghazy T, Weise M, Ebner B, Tugtekin SM, et al. Isolated rupture of the right upper pulmonary vein: a blunt cardiac trauma case. Ann Thorac Surg 2011;91:1267–9.ArticlePubMed
- 7. Yousef R, Carr JA. Blunt cardiac trauma: a review of the current knowledge and management. Ann Thorac Surg 2014;98:1134–40.ArticlePubMed
- 8. Le Guyader A, Bertin F, Laskar M, Cornu E. Blunt chest trauma: a right pulmonary vein rupture. Eur J Cardiothorac Surg 2001;20:1054–6.ArticlePubMed
- 9. Osaka M, Nagai R, Koishizawa T. Rupture of the right upper pulmonary vein and left atrium caused by blunt chest trauma. Gen Thorac Cardiovasc Surg 2017;65:646–9.ArticlePubMed
- 10. Nwaejike N, Mosca R, Hooper TL, Soon SY. Surgical repair of pulmonary vein injury from blunt trauma. Ann R Coll Surg Engl 2015;97:e34–6.ArticlePubMedPMC
- 11. Varghese D, Patel H, Cameron EW, Robson M. Repair of pulmonary vein rupture after deceleration injury. Ann Thorac Surg 2000;70:656–8.ArticlePubMed
- 12. Fukunaga N, Konishi Y, Murashita T, Yuzaki M, Shomura Y, Koyama T, et al. Survival after simultaneous repair of bichamber cardiac and pulmonary vein rupture caused by blunt chest trauma. Ann Thorac Surg 2012;94:265–7.ArticlePubMed
- 13. Nan YY, Lu MS, Liu KS, Huang YK, Tsai FC, Chu JJ, et al. Blunt traumatic cardiac rupture: therapeutic options and outcomes. Injury 2009;40:938–45.ArticlePubMed
- 14. Brathwaite CE, Rodriguez A, Turney SZ, Dunham CM, Cowley R. Blunt traumatic cardiac rupture: a 5-year experience. Ann Surg 1990;212:701–4.ArticlePubMedPMC
- 15. Fulda G, Brathwaite CE, Rodriguez A, Turney SZ, Dunham CM, Cowley RA. Blunt traumatic rupture of the heart and pericardium: a ten-year experience (1979-1989). J Trauma 1991;31:167–73.ArticlePubMed
References
Figure & Data
References
Citations

- The role and timing of cardiopulmonary bypass in the surgical repair of traumatic cardiac injury
Mayo Kondo, Shinichi Ijuin, Tomonori Haraguchi, So Izumi, Reiko Kanno, Kazunori Sakaguchi, Kazumasa Edono, Haruki Nakayama, Satoshi Ishihara, Takuro Tsukube
General Thoracic and Cardiovascular Surgery.2023; 71(10): 561. CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite





