The use of platelet-rich plasma in management of musculoskeletal pain: a narrative review
Article information
Abstract
Musculoskeletal pain is the most common pain reported by patients. Platelet-rich plasma (PRP) is widely used to treat musculoskeletal pain. However, the efficacy of PRP to treat this pain remains controversial. This review highlights the application of PRP in the treatment of musculoskeletal pain. PRP treatment appears to reduce pain and improve function in patients with musculoskeletal pain. However, there are limitations to the currently published studies. These limitations include the PRP preparation methods, type of activators, types of pathology to be treated, methods and times of administration, and association of PRP with other treatments.
Introduction
Among clinically associated pain conditions, musculoskeletal (MSK) pain is the most frequent [1]. MSK diseases are the most common cause of severe long-term pain and physical disability and have a major impact on the quality of life of patients [2,3]. MSK pain affects hundreds of millions of people around the world [4].
The primary goal of physiatrists is to optimize the pain management of their patients with various MSK conditions, including acute and chronic muscle, tendon, ligament, and cartilage disorders. The traditional management of MSK pain involves control with conservative “Rest, Ice, Compression, Elevation” treatment and physical therapy to corticosteroid injections coupled with specific rehabilitation exercises [5].
Although the traditional management of MSK pain may be helpful for short-term pain reduction and early recovery of function, it does not typically reverse the structural changes associated with degenerative conditions. Recently, the multidisciplinary field of tissue engineering has been expanding to enhance healing and stimulate growth in injuries of soft tissue and bone [6].
Platelet-rich plasma (PRP) is one research area that has developed rapidly in recent years. Historically, hematologists coined the term PRP in the 1970s, and platelets have been used to treat patients with hemorrhage or thrombocytopenia [6,7]. The clinical use of PRP as a cell and tissue engineering therapy has dramatically increased over the last decade [8].
PRP is a biological product defined as the plasma fraction of autologous blood with a platelet concentration above baseline after centrifugation [9]. PRP contains many biologically active factors such as platelet-derived growth factor, transforming growth factor-beta (TGF-β), insulin-like growth factor, vascular endothelial growth factor, and epidermal growth factor [10]. PRP concentrates can promote the supraphysiological release of growth factors to enhance healing in chronic injuries, accelerate the acute injury repair process, and reduce MSK pain [11].
Platelet-rich plasma
PRP is defined as the plasma fraction of autologous blood with a platelet concentration above baseline after centrifugation [9]. Platelets are irregularly shaped, non-nucleated cytoplasmic bodies derived from fragmentation of megakaryocyte precursors. Platelets are important in blood clot formation, thrombosis and hemostasis, immunity, inflammation, wound healing, hematological malignancies, and metabolic disorders [12].
PRP contains growth factors that promote cellular anabolism and enhance the release of inflammatory mediators and modulators that exert anti-inflammatory and analgesic effects [13]. PRP counteracts the inflammatory cascade [14]. PRP treatment has been shown to induce the release of hepatocyte growth factor (HGF), a major anti-inflammatory factor. Growth factors (HGF, interleukin-4, and tumor necrosis factor-alpha [TNF-α]) reduce the levels of cyclooxygenase (COX)-1, COX-2, and prostaglandin E2, which are proinflammatory mediators. Additionally, PRP can suppress the production of nuclear factor kappa-light-chain-enhancer of activated B cells, which is highly relevant in soft tissue inflammation [15,16].
PRP promotes tissue regeneration and has gained popularity in recent decades [16]. PRP can induce the production of collagen and growth factors and might increase stem cell numbers, which consequently promotes the healing process by delivering high concentrations of alpha-granules containing biologically active moieties (such as vascular endothelial growth factor and TGF-β) to areas of soft tissue damage [17]. PRP also stimulates cell proliferation and cartilaginous matrix production by chondrocytes and adult mesenchymal stem cells (MSCs). Findings from current clinical trials suggest that PRP has the potential to enhance cartilage repair, attenuate arthritis symptoms, and improve joint function with an acceptable safety profile [13].
Composition of platelet-rich plasma
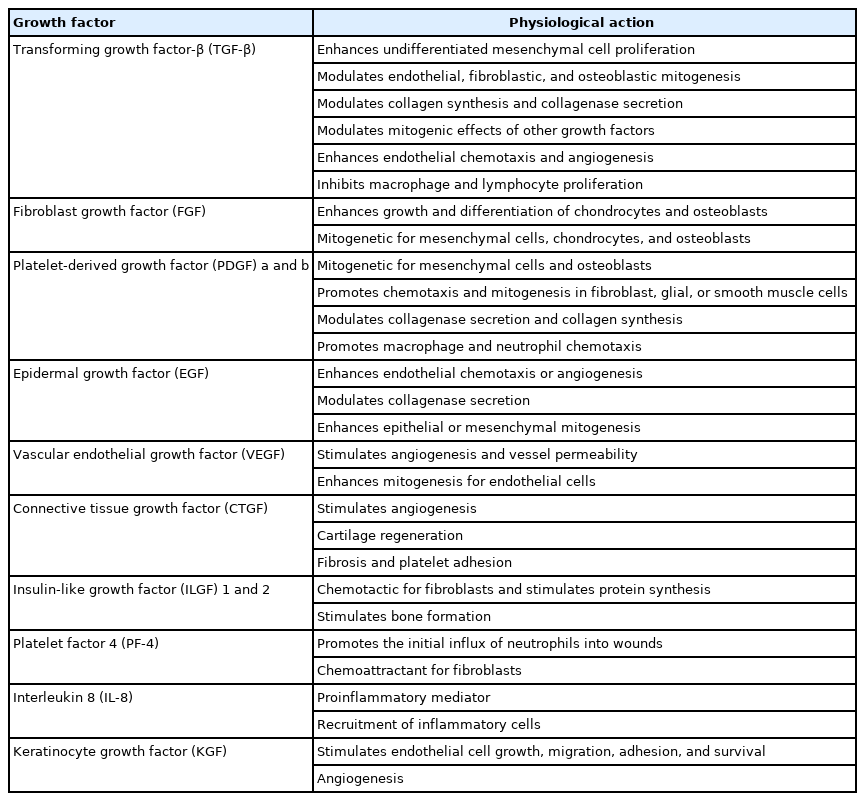
PRP is the plasma from autologous blood after centrifugation and contains a rich concentration of platelets and a variety of growth factors, cytokines, chemokines, and proteins [18]. The key growth factors in PRP are summarized in Table 1. The composition of growth factors promotes tissue repair and regeneration, enhances angiogenesis, and plays a vital role in anti-inflammatory and analgesic effects [19].
Knee osteoarthritis
Symptomatic knee osteoarthritis (OA) is a leading cause of disability globally with a significant financial impact [20]. The development of knee OA involves not only the cartilage but also the entire joint, with changes in the articular bone, synovial membrane, joint capsule, ligaments, and musculature around the joint [21].
There is no disease-modifying therapy for the management of OA; therefore, the treatment goals are to improve pain and function. Pharmacotherapy management includes topical and oral nonsteroidal anti-inflammatory drugs, duloxetine, and periodic intra-articular glucocorticoid and hyaluronan injections [22].
PRP containing growth factors stimulates local angiogenesis, regulates inflammation, inhibits catabolic enzymes and cytokines, and recruits local stem cells and fibroblasts to the damaged sites. PRP also induces nearby healthy cells to synthesize greater amounts of growth factors and increase endogenous hyaluronan synthesis with few serious side effects [23-26]. In recent years, PRP has emerged as a viable treatment method for the management of knee OA [27]. Eighteen studies (all level 1) involving 811 patients undergoing intra-articular PRP injection (mean age, 57.6 years) and 797 patients undergoing hyaluronic acid injection (mean age, 59.3 years) showed that the mean improvement in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) total scores was significantly higher in the PRP group (44.7%) than in the hyaluronic acid group (12.6%) (p<0.01) [28].
Many systematic reviews and meta-analyses have found positive results for PRP in relieving pain and improving function in knee OA [27-30]. Therefore, PRP can be expected to improve pain and function in the management of knee OA, although further studies are needed for the definitive assessment of knee OA treatment.
Ankle joint osteoarthritis
Ankle OA is rarer than OA of the hip and knee and is more common in young active individuals, with a prevalence of 3.4% in the general adult population [31,32]. The primary etiology of ankle OA is trauma, and the overall risk of developing posttraumatic ankle OA after 20 years is almost 40%. The management of ankle OA involves nonsurgical options (medications, physical therapy, orthotics and insoles, and intra-articular injections) and surgical options (joint-sparing surgery, total ankle arthroplasty, and ankle arthrodesis) [33].
Individuals with ankle OA, hemophilic arthropathy, and rheumatoid arthritis were included in 27 studies (1,085 patients). Most of these studies were observational. A case series found that PRP, MSC, hyaluronic acid, and corticosteroid injections provided symptomatic relief, although the efficacy of corticosteroid injections was short-term [34].
PRP injections for ankle OA are valid and safe alternatives for postponing the need for surgery [31]. PRP injections are favored for the treatment of pain associated with ankle OA. However, the relative efficacy of PRP injection therapy is far from definitive and warrants further high-quality comparative trials [34].
Temporomandibular joint osteoarthritis
The prevalence of temporomandibular (TM) joint OA is increasing, and it is more common in women. OA may cause pain in the TM joint area [35,36]. Excessive or prolonged overload of TM joints may lead to adverse remodeling, resulting in OA. The management of TM OA includes conservative treatment (medications, splints, and physiotherapy), intra-articular injections, arthrocentesis, arthroscopy, and open-joint surgery [37].
A comparative randomized study showed that maximum improvements in pain-free mouth opening and reduction in pain severity were observed in all groups (bite splint, betamethasone, sodium hyaluronate, and PRP injections in addition to using the bite splint). In the PRP group, patients with a maximum pain-free mouth opening value of 25.8 mm before treatment improved to 46.8 mm after treatment. The PRP group showed the best results after 6 months [38].
PRP injections may reduce pain and joint sound and improve the range of motion of the TM joint because PRP injections have anti-inflammatory and analgesic properties. PRP restores intra-articular hyaluronic acid levels, increases chondrocyte glycosaminoglycan synthesis, and balances joint angiogenesis. However, a standardized protocol for PRP preparation and application needs to be established [37-40].
Low back pain
Low back pain (LBP) involves a spectrum of different types of pain (e.g., nociceptive, neuropathic, nociplastic, and nonspecific) that frequently overlap. LBP can be caused by lumbar spine elements (e.g., soft tissue, vertebrae, zygapophyseal and sacroiliac joints, intervertebral discs, and neurovascular structures) [41]. Therapy for LBP usually begins with self-care and medication in combination with non-pharmacological methods, such as physical therapy and psychological treatment, in appropriate patients [42].
Systematic reviews and single-arm meta-analyses showed that PRP may be effective in managing discogenic LBP, radicular pain, facet joint pain, and sacroiliac joint pain. However, the levels of evidence vary [43,44]. Intradiscal PRP injections can be a safe, inexpensive, and feasible treatment to counter the intervertebral disc degeneration associated with LBP. It is important to administer PRP early during the course of treatment to stimulate growth of the remaining cells in the disc [45,46]. PRP injections in the lumbar multifidus muscle can be a safe and inexpensive approach to treating LBP [47]. A small number of prospective trials have described that PRP injection may improve the pain or functional decline caused by facet joint arthropathy for a longer duration [48].
In 2017, a prospective comparative study including 46 patients showed statistically significant pain reduction in both groups (PRP, group A and corticosteroid/local anesthesia, group B). However, for subjective satisfaction based on the modified MacNab criteria, the success rate for group B remained at 20% after 6 months, while it increased over time in group A. Therefore, autologous PRP was suggested as a superior treatment option for long-duration efficacy in lumbar facet joint syndrome [49].
Twenty patients completed another prospective clinical trial. The improvements in pain scores (numerical rating scale and Oswestry Disability Index scores) were positively correlated with platelet concentrations in the PRP group [46].
In conclusion, the use of PRP in various injections, such as intradiscal, intrafacet, and intramuscular injections, has yielded significantly reduced pain and improved patient satisfaction, with a significant advantage of no major complications. However, further studies with larger sample sizes and control groups are needed to confirm its efficacy [43,44,48,50].
Myofascial pain syndrome
Myofascial pain is an important cause of disability in the whole population [51]. Emerging symptoms arise from each painful myofascial trigger point, which is a hypersensitive spot within a taut band of skeletal muscle that produces pain on compression, stretch, overload, or contraction of the tissue. The end result is usually pain that is perceived to be distant from the spot of origin. In a randomized controlled trial, there was no statistically significant difference in pain levels between the “lidocaine” and “PRP” groups before and 2 weeks after treatment; however, a statistically significant difference was found between the two groups 4 weeks after treatment (p<0.001). Specifically, 4 weeks after the injection, the average pain of the patients in the lidocaine and PRP groups was 3.4 and 0.9 on the visual analogue scale (VAS), respectively [52].
There are a few studies associated with myofascial pain that were conducted only on the masticatory muscles, which are involved in the most common TM disorders. PRP injections effectively improved trigger-point symptoms in the masseter muscle at 1 and 3 months [52,53].
Lateral epicondylitis
As tendons have poor vascularity, the tissue has limited healing and the lesions are not reversible, resulting in tendinopathies due to trauma or excessive overload. This causes tendon soreness, reduced strength, pain upon exertion, and progressive reduction in function [54].
Lateral epicondylitis, also known as tennis elbow, is a common musculotendinous degenerative disorder of the extensor origin at the lateral humeral epicondyle in adults [55], with a prevalence of 1% to 3% in the general population [56]. The presenting symptoms include lateral elbow pain, pain caused by wrist extension, and weakened grip strength. The diagnosis is always made clinically through medical history and physical examinations [57]. The treatment of lateral epicondylitis includes rest, nonsteroidal anti-inflammatory medication, bracing, physical therapy, extracorporeal shock wave therapy (ESWT), and botulinum toxin injection [58].
Compared with lateral epicondyle surgery, PRP injections provide similar improvements in pain and function in patients suffering from lateral epicondylitis [59]. PRP components promote cell recruitment, proliferation, and angiogenesis. It has also been suggested that PRP induces a transient inflammatory response, resulting in a regenerative response and immunomodulatory effects on tenocytes [60].
A randomized study involving 83 patients was conducted in 2007. The study was composed of two groups: group A, local steroid injection (n=50) and group B, autologous PRP (n=33). A significant difference between the two groups (p=0.0001) was found in pain and function at the end of 6 months. Group B showed a 91% mean improvement (8.33–0.69) in VAS score compared to a 42.2% mean improvement (7.98–4.61) in group A. Regarding function assessment, MAYO Elbow Scores also indicated a favorable outcome in the PRP-treated patients (group B) with a 54.4% mean improvement (61.51–95.0) compared to a 1.25% mean improvement (63.92–63.12) in the steroid-treated patients (group A), a difference that was statistically significant (p=0.0001) [61].
Many systematic reviews and meta-analyses have found that PRP can be considered a safe and effective treatment option for lateral epicondylitis with clinical improvements in pain and function, although there is a lack of quantification of specific PRP content and considerable heterogeneity among randomized controlled trials exists [62-65].
Plantar fasciitis
Plantar fasciitis is a common cause of heel pain and is associated with significant morbidity. It is a debilitating degenerative condition of the plantar fascia resulting from repetitive microtrauma and excessive strain on the plantar surface of the foot [66]. PRP may modulate plantar fascia degeneration because of its regenerative properties [67]. PRP also releases vascular endothelial growth factor, which increases angiogenesis and may facilitate the healing of degenerative conditions by promoting neovascularization and repair [68].
PRP has been suggested as a safe therapeutic option in the treatment of plantar fasciitis, as it reduces pain and improves function in patients with this condition, and its effect persists long term [69-71].
Patellar tendinopathy (jumper’s knee)
Patellar tendinopathy (PT) is referred to as “jumper’s knee,” a clinical and chronic overuse condition of unknown pathogenesis and etiology [72]. A large proportion of patients are refractory to conservative treatment, and a variety of new treatments have emerged, including PRP injections [73]. PRP-containing growth factors have been shown to play a role in tendon healing [74,75]. The growth factors in PRP have been observed to play crucial roles in the tissue healing process, collagen production, and tendon cell proliferation [76].
To compare PRP with focused ESWT among athletes with chronic PT, a randomized controlled single-center trial with 12 months of follow-up was performed. During the 12-month follow-up period, the Victorian Institute of Sport Assessment-Patella questionnaire scores for both groups improved significantly from baseline (55.3 for PRP, 56.1 for ESWT), although the PRP group showed greater improvement at 6 months (86.7 vs. 73.7, p=0.014) and 12 months (91.3 vs. 77.6, p=0.026). The pain scores during five single-leg squats demonstrated similar trends. At 12 months, a greater proportion of patients in the PRP group rated their response to treatment as good or excellent (PRP, 91.3% vs. ESWT, 60.8%; p=0.035) [77].
Therefore, PRP plays a potential role in the treatment of PT, leading to a significant decrease in pain and significant improvement in knee function and quality of life over 12 months [78-82].
Rotator cuff tendinopathy
More than 50% of all shoulder pain cases are considered to be related to tendinopathies of the rotator cuff (RC), such as tendinosis and incomplete thickness tears of the supraspinatus [81]. In the management of RC tendinopathy, physical rehabilitation, rest, and nonsteroidal anti-inflammatory drugs are considered conventional treatments; however, the best treatment is still inconclusive [83,84].
PRP has been reported to promote the proliferation of two tendon cell types; tenocytes and tendon stem/progenitor cells. Several studies have shown that PRP can induce tenocyte proliferation in vitro [85].
For patients with RC tendinopathy, corticosteroids yield pain reduction and functional improvement in the short term (3–6 weeks), but not in the long term (over 24 weeks). In contrast, PRP may yield better long-term outcomes (more than 24 weeks) [86].
Moreover, the long-term retear rates of RC-related abnormalities were significantly decreased in patients who received PRP [87].
Many systematic reviews and meta-analyses have found that the currently available clinical evidence on PRP injections supports a beneficial effect on pain reduction and functional outcomes in RC tendinopathy [88-91].
Adhesive capsulitis
Adhesive capsulitis (AC) of the shoulder is a common clinical condition characterized by insidious and progressive pain resulting in loss of glenohumeral joint function [92]. However, the etiology of AC remains unclear. It has been postulated that the motion limitations of the shoulder joint are due to an imbalance between fibrosis and loss of normal collagenous remodeling after an inflammatory healing response [93].
PRP can exert an anti-inflammatory effect at the inflammation site by releasing TNF-α, HGF, and lipoxin A4, which are potent anti-inflammatory agents [94,95].
At the 12-week follow-up in another study, a single injection of PRP was found to be more effective than corticosteroid injection in improving pain, disability, and shoulder range of movement in patients with AC [96].
PRP injections have been found to be effective in reducing pain and improving shoulder joint function due to AC [93,96,97]. These findings suggest that PRP is a therapeutic option for the management of AC.
Adverse effects
The most common adverse effect was mild pain and discomfort at the injection site after PRP injection [98]. Some authors have reported that PRP injections are more painful than saline injections. However, no serious adverse effects were observed [99].
Limitations
Although good clinical outcomes and safety profiles can be achieved with the use of PRP, there are discrepancies in the existing literature. Several variables must be considered when using PRP. However, these variables were not described herein. PRP preparation methods, types of activators, types of pathology to be treated, routes and times of administration, and the association of PRP with other treatments can influence outcomes. Although several research articles have been published on PRP, this field still requires more scrutiny because of the inconsistent results of different studies, and a definite direction remains elusive.
Conclusion
This review article presents available evidence supporting the clinical efficacy of PRP in patients with MSK pain, with fewer side effects. PRP leads to reductions in pain and improvements in patient's function; however, evidence to clarify the discrepancies in PRP therapy is still needed.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.