PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 36(3); 2019 > Article
-
Case report
Late complication of the Nuss procedure: recurrent cardiac tamponade -
Won Jong Park1
 , Jang Won Son2
, Jang Won Son2 , Kyu Hwan Park3
, Kyu Hwan Park3 , You Min Kim4
, You Min Kim4 , Jong Ho Nam2
, Jong Ho Nam2 , Kang Un Choi5
, Kang Un Choi5 , Jung Ho Kim6
, Jung Ho Kim6
-
Yeungnam University Journal of Medicine 2019;36(3):260-264.
DOI: https://doi.org/10.12701/yujm.2019.00241
Published online: June 13, 2019
1Division of Cardiology, Department of Internal Medicine, Dong-Eui Medical Center, Busan, Korea
2Division of Cardiology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
3Division of Cardiology, Department of Internal Medicine, Daegu Veterans Hospital, Daegu, Korea
4Division of Cardiology, Department of Internal Medicine, Pohang SM Christianity Hospital, Pohang, Korea
5Division of Cardiology, Department of Internal Medicine, Dongguk University Gyeongju Hospital, Gyeongju, Korea
6Department of Emergency Medicine, Yeungnam University Medical Center, Daegu, Korea
- Corresponding author: Jang Won Son, Division of Cardiology, Department of Internal Medicine, Yeungnam University College of Medicine, 170, Hyunchung-ro, Nam-gu, Daegu 42415, Korea Tel: +82-53-620-3314, Fax: +82-53-621-3310, E-mail: gubjae@hanmail.net
Copyright © 2019 Yeungnam University College of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 6,302 Views
- 68 Download
Abstract
- Pectus excavatum (PE) is known as one of the most common congenital deformities of the anterior chest wall. The Nuss procedure is an effective surgical therapy to correct PE. Here, we report a case of recurrent cardiac tamponade due to hemopericardium that occurred after 16 months following the Nuss procedure. The cause of recurrent hemopericardium was thought to be local, repetitive irritation of the pericardium by the Nuss steel bar. We should keep in mind that this serious complication can occur after the Nuss procedure, even in the late phase.
- Pectus excavatum (PE) is one of the most common congenital chest wall deformities, occurring in approximately 1:400 births and affecting males 5 times more often than females [1]. Patients with PE may have a variety of symptoms, such as nonspecific chest pain, shortness of breath on exertion, and psychological distress, which are the indications of surgical treatment.
- There are two standard surgical therapies of PE: the Ravich procedure, corrective osteotomy, and the Nuss procedure, minimally invasive repair of PE using the Nuss bar. The Nuss procedure has become a widely used method correcting PE since Dr. Donald Nuss introduced it in 1998, with benefits including being a minimally invasive technique and having a short operative duration [2]. This procedure elevates the depressed sternum by passing a suitably shaped, concave steel bar beneath the sternum, resting on the outer aspects of the ribs on each side under thoracoscopic guidance [3]. Pericarditis or pericardial effusions as one of the postoperative complications have been reported in 1.6–2.4% of cases [4-6], but progression to cardiac tamponade is very rare.
- Here, we introduce an instructive case which gives us meaningful messages that cardiac tamponade can occur as a late complication of the Nuss procedure.
Introduction
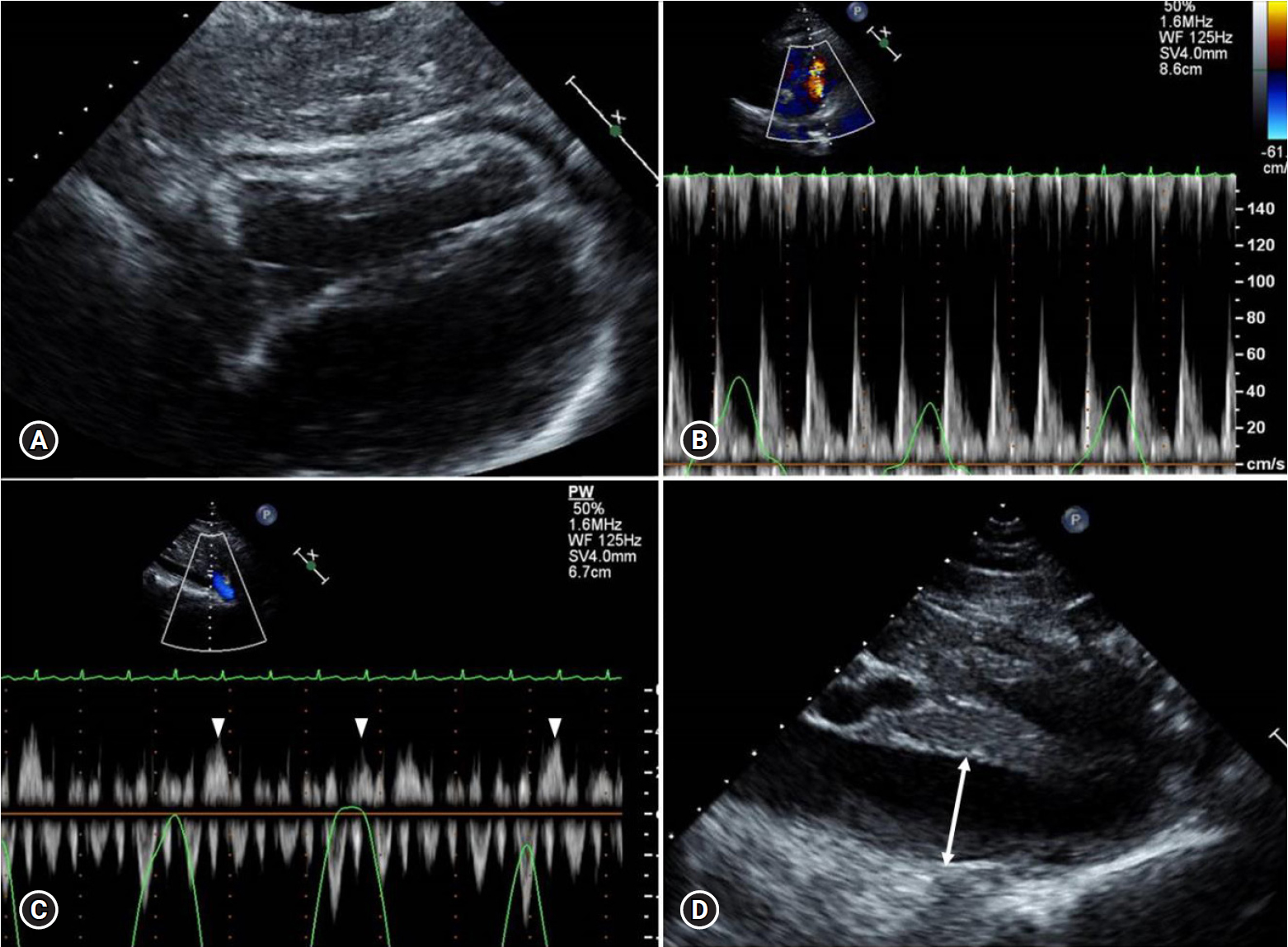
- A 23-year-old woman visited the emergency department with the chief complaint of chest discomfort with a burning sensation on the anterior chest, aggravated by inspiration or bending forward. She was a university student majoring in vocal and got the Nuss procedure 16 months ago to correct PE for increasing lung capacity. Her blood pressure (BP) was 105/65 mmHg with a heart rate of 128 beats/min (bpm), and her respiration rate was 22 breaths/min and body temperature was 36.9°C. On physical examination, her neck veins were distended, and her lower extremities were swollen with pitting edema. Lung sounds were clear, but her heart sound was mildly decreased on auscultation. A chest X-ray showed a well-positioned Nuss bar without any pathologic finding, laboratory finding, nor any abnormalities. Electrocardiogram showed a low voltage QRS. Trans-thoracic echocardiography (TTE) revealed a moderate amount of pericardial effusion with diastolic collapse of the right ventricle, more than 25% of respiratory variation of mitral inflow velocity, expiratory diastolic hepatic vein flow reversal, and dilated inferior vena cava (IVC) with plethora, which were all compatible hemodynamic findings for cardiac tamponade (Fig. 1).
- Emergent TTE and fluoroscopy-guided pericardiocentesis were performed through a subxiphoid approach, and 700 mL of bloody effusion was drained. The pericardial fluid analysis revealed exudate with a hemoglobin of 12.2 g/dL and an adenosine deaminase (ADA) of 36.7 mg/dL. Chest computed tomography (CT) was performed to rule out disorders that can cause hemopericardium, but there was no evidence of acute aortic syndrome such as aortic dissection and no abnormal malignant mass or lung infiltration. The pericardial tube was removed on hospital day 5 and follow-up echocardiography showed a nearly disappeared pericardial effusion.
- Bloody pericardial effusion had a high ADA level and, considering the high incidence of tuberculous pericarditis in South Korea, the etiology of pericardial effusion was assumed to be tuberculous pericarditis, and anti-tuberculous medications were started on hospital day 8. The patient discharged without any further events and followed up at the outpatient department free of symptoms.
- However, after 2 months, she visited our emergency department again with similar symptoms as on her first visit. Her initial vital sign showed a BP of 136/87 mmHg with a heart rate of 128 bpm, but 4 hours later, her BP abruptly decreased to 60/40 mmHg. Emergent bedside echocardiography was performed and revealed a small amount of pericardial effusion. Even though the amount was small, 2-dimentional and Doppler studies demonstrated significant tamponade physiology, including septal bouncing motion, more than 25% of the respiratory variation of mitral inflow, expiratory diastolic hepatic vein flow reversal, and dilated IVC with a plethora (Fig. 2). Considering recurrent pericardial effusion, even on the anti-tuberculous medication, we tried to find another etiology other than tuberculous pericarditis. We carefully reviewed the chest CT and recognized that the Nuss bar is contacting with the pericardium (Fig. 3). We inferred that the friction between the Nuss bar and pericardium can make hemopericardium, and it could be the main culprit of recurrent cardiac tamponade in this patient. The amount of pericardial effusion was too small to perform pericardiocentesis, and elimination of the Nuss bar was needed to prevent recurrent tamponade, so we made a decision to have an emergency operation of a pericardial window formation and removal of the Nuss bar at the same time. About 200 mL of bloody pericardial effusion was drained by window formation, and the Nuss bar was successfully removed. There was no perforation or injuries to the pericardium or great vessels. Her central venous pressure decreased from 14 to 7 mmHg after the window formation, and her BP recovered to normal range.
- On the fourth postoperative day, the pericardial effusion almost disappeared upon echocardiography. Interferon-gamma release assays, polymerase chain reaction testing for tuberculosis, and mycobacterial culture of pericardial fluid were all negative and anti-tuberculous medications were stopped. She discharged without any specific complications on hospital day 17, and follow-up echocardiography at 6 months did not show any abnormal findings.
Case
- The Nuss procedure is one of the well-established operation techniques for correcting PE [2]. Although some authors developed a variety of sternal-lifting methods to improve the visual field and to increase the space under the substernal area minimizing the risk of cardiac injury during and after surgery [5,7], cardiac complications have occurred in real clinical fields.
- In general, complications caused by the Ravitch procedure and Nuss bar implantation can be classified as acute and chronic complications, based on 30 days after the surgical procedure [8,9], and life-threatening events, such as cardiac perforation and other direct heart or aortic injuries have mostly occurred acutely during still bar placement. Pericarditis and pericardial effusion are rare complications that can develop later; however, progression to life-threatening cardiac tamponade is extremely rare [4-6]. The cases presented with tamponade were mostly related to sternal wire after the Ravitch procedure [10-12] or Nuss bar displacement injuring the ascending aorta [13] or pericardium [14].
- To our best knowledge, this is the first case report of very late spontaneous cardiac tamponade, without evidence of Nuss bar displacement. In our case, there was no evidence of visible traumatic injury at great vessels and the pericardium on the chest CT scan and surgical field during a window formation of the pericardium. There was also no other foreign body or metal wire, which can cause a direct injury to the pericardium. Referring to literature from Yang et al. [14], we thought that the reason of recurrent, late-onset cardiac tamponade after the Nuss procedure is due to micro-bleeding of small vessels around the pericardium into the pericardial space caused by local, repetitive irritation of the pericardium by the Nuss steel bar. After the removal of the bar, there had been no pericardial effusions upon follow-up TTE in the outpatient clinic.
- Another important instruction we learned from this case was that only 200 mL of a very small amount of pericardial effusion can cause life-threatening cardiac tamponade if it accumulates rapidly (Fig. 3). Rapidly increasing pericardial fluid first reaches the limit of the pericardial reserve volume and then quickly exceeds the limit of parietal pericardial stretch, causing a steep rise in intra-pericardial pressure, subsequently developing cardiac tamponade [15-17].
- Those who have a Nuss bar or other foreign devices adjacent to the heart presenting with pericardial effusion should be considered for the possibility of hemopericardium and cardiac tamponade related to the device, and only small pericardial effusions can induce cardiac tamponade if it accumulates rapidly over the compensatory mechanism of the pericardium.
Discussion


- 1. Jaroszewski DE, Fonkalsrud EW. Repair of pectus chest deformities in 320 adult patients: 21 year experience. Ann Thorac Surg 2007;84:429–33.ArticlePubMed
- 2. Nuss D, Kelly RE Jr, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545–52.ArticlePubMed
- 3. Krasopoulos G, Goldstraw P. Minimally invasive repair of pectus excavatum deformity. Eur J Cardiothorac Surg 2011;39:149–58.ArticlePubMedPDF
- 4. Žganjer M, Žganjer V. Surgical correction of the funnel chest deformity in children. Int Orthop 2011;35:1043–8.ArticlePubMedPDF
- 5. Yoon YS, Kim HK, Choi YS, Kim K, Shim YM, Kim J. A modified Nuss procedure for late adolescent and adult pectus excavatum. World J Surg 2010;34:1475–80.ArticlePubMedPDF
- 6. Park HJ, Lee SY, Lee CS, Youm W, Lee KR. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg 2004;77:289–95.ArticlePubMed
- 7. Johnson WR, Fedor D, Singhal S. A novel approach to eliminate cardiac perforation in the Nuss procedure. Ann Thorac Surg 2013;95:1109–11.ArticlePubMed
- 8. Kelly RE Jr, Mellins RB, Shamberger RC, Mitchell KK, Lawson ML, Oldham KT, et al. Multicenter study of pectus excavatum, final report: complications, static/exercise pulmonary function, and anatomic outcomes. J Am Coll Surg 2013;217:1080–9.ArticlePubMed
- 9. Fallon SC, Slater BJ, Nuchtern JG, Cass DL, Kim ES, Lopez ME, et al. Complications related to the Nuss procedure: minimizing risk with operative technique. J Pediatr Surg 2013;48:1044–8.ArticlePubMed
- 10. Barakat MJ, Morgan JA. Haemopericardium causing cardiac tamponade: a late complication of pectus excavatum repair. Heart 2004;90:e22.ArticlePubMedPMC
- 11. Cope SA, Rodda J. Cardiac tamponade presenting to the emergency department after sternal wire disruption. Emerg Med J 2004;21:389–90.ArticlePubMedPMC
- 12. Lee SH, Cho BS, Kim SJ, Lee SY, Kang MH, Han GS, et al. Cardiac tamponade caused by broken sternal wire after pectus excavatum repair: a case report. Ann Thorac Cardiovasc Surg 2013;19:52–4.ArticlePubMed
- 13. Hoel TN, Rein KA, Svennevig JL. A life-threatening complication of the Nuss procedure for pectus excavatum. Ann Thorac Surg 2006;81:370–2.ArticlePubMed
- 14. Yang MH, Cheng YL, Tsai CS, Li CY. Delayed cardiac tamponade after the Nuss procedure for pectus excavatum: a case report and simple management. Heart Surg Forum 2008;11:E129–31.ArticlePubMed
- 15. Spodick DH. Acute cardiac tamponade. N Engl J Med 2003;349:684–90.ArticlePubMed
- 16. Gascho JA, Martins JB, Marcus ML, Kerber RE. Effects of volume expansion and vasodilators in acute pericardial tamponade. Am J Physiol 1981;240:H49–53.ArticlePubMed
- 17. Spodick DH. The normal and diseased pericardium: current concepts of pericardial physiology, diagnosis and treatment. J Am Coll Cardiol 1983;1:240–51.ArticlePubMed
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite




