PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 39(3); 2022 > Article
-
Original article
Effect of nonsurgical periodontal therapy and smoking status on hematological variables related to anemia of chronic disease in chronic periodontitis patient: a case-control study -
Sangita Show1
 , Somen Bagchi2
, Somen Bagchi2 , Arka Kanti Dey3
, Arka Kanti Dey3 , Ramanarayana Boyapati4
, Ramanarayana Boyapati4 , Pritish Chandra Pal5
, Pritish Chandra Pal5 , Kanikanti Siva Tejaswi4
, Kanikanti Siva Tejaswi4
-
Journal of Yeungnam Medical Science 2022;39(3):244-249.
DOI: https://doi.org/10.12701/jyms.2022.00045
Published online: May 16, 2022
1Department of Periodontology, Trinity Dental & Maxillofacial Multispeciality Clinic, Kolkata, India
2Department of Periodontics, Dr. R. Ahmed Dental College and Hospital, Kolkata, India
3Department of Oral and Maxillofacial Surgery, Diamond Harbour Government Medical College and Hospital, Diamond Harbour, India
4Department of Periodontology, Sibar Institute of Dental Sciences, Guntur, India
5Department of Periodontology, Pacific Dental College and Hospital, Udaipur, India
- Corresponding author: Sangita Show, MDS Department of Periodontology, Trinity Dental & Maxillofacial Multispeciality Clinic, 2/C R.N Tagore Road, Budge Budge, Kolkata, West Bengal 700137, India Tel: +91-83-2741-3017 • Fax: +91-33-2265-6876 • E-amil: sangitashow739@gmail.com
Copyright © 2022 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,703 Views
- 83 Download
Abstract
-
Background
- Chronic infectious, inflammatory, or neoplastic disorders are associated with anemia of chronic disease. Chronic inflammatory diseases such as periodontitis may contribute to masked anemia, especially in smokers. This study was aimed at verifying and comparing the efficacy of nonsurgical periodontal therapy (NSPT) for improving anemia among chronic periodontitis patients with and without the habit of smoking.
-
Methods
- Thirty systemically healthy individuals with chronic periodontitis were divided into two groups of 15 each, smokers (group A) and nonsmokers (group B). The groups were compared based on hematological parameters such as serum erythropoietin (SE) and serum ferritin (SF) levels at baseline and 3 months after NSPT for anemia evaluation.
-
Results
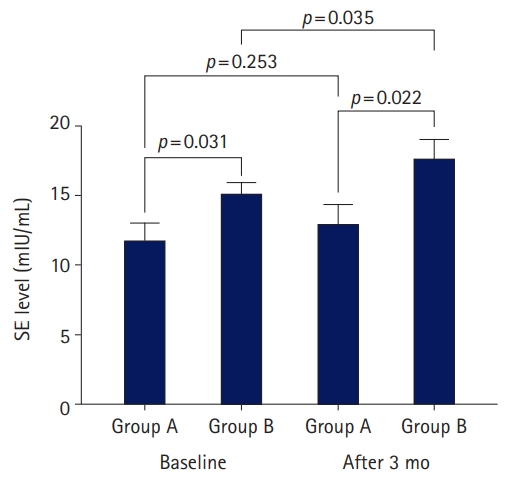
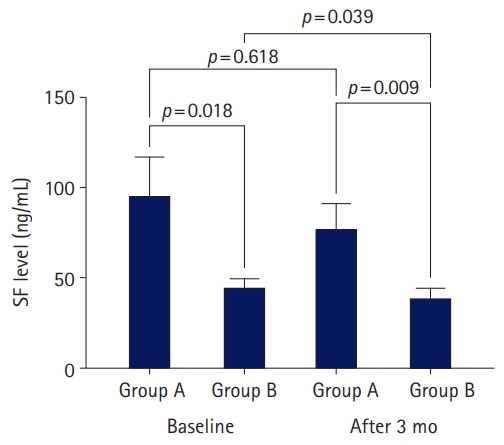
- The baseline SE levels in groups A and B were 11.84 and 15.19 mIU/mL (p=0.031), respectively; the corresponding levels at 3 months after NSPT were 13.00 and 17.74 mIU/mL (p=0.022). The baseline SF levels in groups A and B were 95.49 and 44.86 ng/mL (p=0.018), respectively; the corresponding levels at 3 months after NSPT were 77.06 and 39.05 ng/mL (p=0.009). Group B showed a significant increase and decrease in the SE and SF levels, respectively, at 3 months after NSPT (p=0.035 and p=0.039, respectively), whereas group A showed insignificant changes (p=0.253 and p=0.618, respectively).
-
Conclusion
- NSPT led to an improvement in anemia among chronic periodontitis patients. However, the improvement is less in smokers compared to that in nonsmokers. Furthermore, SF and SE levels might serve as effective biomarkers for assessing anemia in smokers and nonsmokers with chronic periodontitis.
- Chronic infectious, inflammatory, or neoplastic disorders are associated with anemia of chronic disease (ACD) [1]. Pathophysiological factors such as limited iron availability to erythroid progenitor cells, a blunted response to erythropoietin, erythrophagocytosis, diminished erythropoiesis, and microbial/tumor cell infiltration of bone marrow contribute to the development of ACDs. Patients with ACD demonstrate diminished levels of serum iron, normal to elevated serum ferritin (SF) levels, and normocytic to microcytic anemia [2]. Periodontitis is a chronic inflammatory disease characterized by increased production of inflammatory cytokines that can contribute to the prevalence of anemia by directly inhibiting erythropoiesis and inducing changes in iron absorption and release [3].
- Patients with chronic periodontitis (CP) who are regular smokers show lower gingival redness and bleeding on probing due to potential vasoconstriction caused by the nicotine content in tobacco. This may lead to an inaccurate assessment of periodontal status and failure to diagnose the underlying pathogenic state [4]. In addition, smoking causes an increase in hemoglobin (Hb) concentration mediated by carbon monoxide, which bonds with Hb and forms inactive carboxyhemoglobin (COHb) with a reduced ability to deliver oxygen to the tissues. Therefore, as a compensatory mechanism, smokers maintain a higher Hb level than nonsmokers, which is referred to as secondary polycythemia [5,6]. Despite the higher Hb levels found in smokers, this hypoxic state triggers erythropoietin production, thereby increasing erythropoiesis. Erythropoietin is a large glycoprotein hormone produced by the peritubular cells lining the kidneys and hepatocytes; it is the principal regulator of the erythrocyte lineage [7]. This clearly implies that the underlying anemic state in smokers is masked by high Hb values, which may lead to an underestimation of the prevalence of anemia among smokers [8]. In such a scenario, an estimation of serum erythropoietin (SE) levels may aid in assessing the anemia status of smokers.
- In chronic inflammatory conditions such as CP, proinflammatory cytokines such as interleukin (IL)-1α, IL-1β, IL-6, tumor necrosis factor-α, and transforming growth factor-β not only increase hemolysis and impair erythropoiesis via direct bone marrow suppressive effects but also release reactive oxygen species that inhibit erythropoietin gene expression [9]. Singh et al. [10] and Hutter et al. [11] found lower erythropoietin levels in patients with CP, thereby strengthening the hypothesis that CP may lead to ACD.
- Acute-phase proteins are biomarkers that show changes in plasma concentration that increase (positive acute-phase proteins), such as ferritin, or decrease (negative acute-phase proteins) by at least 25% during inflammatory disorders, due to their altered production by hepatocytes [12]. Ferritin serves as the main iron storage protein in the body and contains 20% iron by weight. The serum iron concentration is directly proportional to its storage in the body, which increases under inflammatory conditions and iron overload. Chakraborty et al. [13] observed that SF levels were higher in patients with CP than in healthy controls, and a reduction was noted with remission of chronic inflammation following nonsurgical periodontal therapy (NSPT). Considering the prevalence of periodontal disease in the community at large, its deleterious effects on the systemic health of affected individuals, the increased use of tobacco in the form of cigarette smoking, and the resultant masking of anemia status, therapeutic measures such as scaling and root planning (both NSPTs) might significantly improve anemia status in such individuals.
- The available literature suggests that NSPTs were not tested while evaluating erythropoietin levels in smokers and nonsmokers with CP. To date, only a few studies have evaluated NSPTs with a single hematological parameter to assess ACD in CP cases. Hence, multiple hematological parameters, such as SF and SE levels, collectively might serve as a better means to assess the anemia status of smokers with CP instead of any single parameter. The aim of the present study was to verify and compare the efficacy of NSPT in improving anemia status among patients with CP who do or do not smoke.
Introduction
- Ethical statements: This study was carried out following CONSORT (Consolidated Standards of Reporting Trials) guidelines and written informed consent was obtained from all participants who fulfilled the inclusion criteria and agreed to participate voluntarily. Details about the nature, risk, and benefits of the hematological investigations as well as the associated procedures were explained to all participants. The experimental protocol and consent form were approved by the Institutional Ethical Committee and Institutional Review Board (IRB) of Dr. R. Ahmed Dental College and Hospital (IRB No: DCH/07/18-19).
- 1. Study design
- This clinico-biochemical study included 30 systemically healthy patients diagnosed with CP stage I/II (probing pocket depth of ≥4 mm but <6 mm) requiring NSPT who were selected from the outpatient Department of Periodontics [14]. CP was confirmed clinically and radiographically according to the guidelines of the 2017 Periodontology Consensus Report [14]. Subjects were divided into two groups (n=15 per group) based on their smoking history. Group A included current smokers (i.e., individuals with a history of smoking ≥100 cigarettes in their lifetime and currently smoking) and group B included never smokers (i.e., individuals who never smoked/history of smoking <100 cigarettes in their lifetime) [15]. Pregnant and lactating mothers, former smokers, and those with any history of systemic illness, history of iron supplements or blood loss, any periodontal surgery in the last 6 months, and pocket depth ≥6 mm were excluded from the study.
- After careful periodontal examination and diagnosis, venous blood samples were obtained in the early morning to avoid diurnal variations in SE levels. Peripheral venous blood (4 mL) was obtained by venipuncture (Mokshy Surgicals Ltd., Mumbai, India) in the antecubital fossa from each participant selected for hematological tests. The blood was transferred to non-vacuum clot activator (coated with micronized silica) blood collection tubes. The collected blood samples were kept at room temperature for approximately 2 hours to allow the blood to clot, and serum was obtained after centrifugation for 10 minutes at 2,500 revolutions per minute (Remi Elektrotechnik Ltd., Thane, India). The serum was then assayed for baseline periodontal and hematological parameters (SF and SE). The selected subjects in both groups then received NSPT, including ultrasonic scaling, root planing, and polishing, as required. Thorough oral hygiene instructions and demonstration of proper brushing technique were provided. The patients were asked to return at 1- and 3-month intervals for follow-up, and additional oral prophylaxis was administered at those times if required. All periodontal interventions were performed by an expert periodontist who was unaware of the specific grouping of the subjects. The final hematological data were recorded at the 3-month follow-up, and statistical analysis of the data was carried out. Oral hygiene was maintained at an optimal level during the study period.
- SF levels were measured using an Access Immunoassay System and analyzed using an automated analyzer (Beckman Coulter Immunoassay System, Brea, CA, USA). SE levels were assessed using an enzyme-linked immunosorbent assay (ELISA) kit for erythropoietin and an Adonis ELISA plate reader system (Triveni Traders & Diagnostic Private Ltd., Thane, India).
- 2. Statistical analysis
- The Shapiro-Wilk test was performed to assess the assumption of normality of the data. Data are presented as mean±standard error of the mean (SEM). An unpaired Student t-test was performed to compare the parameters of the two groups that showed normal distributions. Normally distributed paired data of each group were compared using a paired Student t-test. Non-normally distributed unpaired data were evaluated using the Mann-Whitney U-test, and paired data were evaluated using the Wilcoxon matched-pairs signed-rank test. Correlations between two normally distributed parameters were evaluated using the Pearson correlation test. Sex distribution between the two groups was evaluated using Fisher exact test. The correlation between two non-normally distributed parameters was evaluated using Spearman nonparametric correlation. Direct and inverse correlations were indicated by positive and negative correlation coefficient (r) values, respectively. An absolute value of r of 1.0 to 0.5, 0.5 to 0.3, 0.3 to 0.1, and <0.1 was considered strong, moderate, weak, and no correlation, respectively. Differences were considered statistically significant at p<0.05. Statistical analysis was performed using Graph Pad Prism ver. 5, 2007 (Graph Pad Software Inc., San Diego, CA, USA).
Methods
- The Shapiro-Wilk test and visual inspection of the histograms and quantile-quantile plots suggested that the collected data were normally distributed. In the present study, the ages (mean±SEM) of the participants in groups A and B were 47.73±2.33 years and 41.93±2.79 years, respectively. An unpaired Student t-test showed that the mean age of the participants was not statistically different between the groups (p=0.122) (Table 1). Regarding sex distribution between the groups, group A had nine male patients and six female patients, and group B had seven male patients and eight female patients. A chi-square test showed that there was no statistically significant difference in the sex distribution (p=0.457). Hence, confounding variables, such as age and sex, did not affect the study results (Table 1). Group B showed higher SE levels than group A both at baseline (group A, 11.84±1.24 mIU/mL and group B, 15.19±0.79 mIU/mL; p=0.031) as well as after 3 months of periodontal intervention (group A, 13.00±1.40 mIU/mL and group B, 17.74±1.36 mIU/mL; p=0.022) (Table 2, Fig. 1). No significant alteration in the SE level was observed in group A (p=0.253) after 3 months of periodontal therapy (Table 2). However, the SE level in group B increased significantly (p=0.035) after 3 months compared to the baseline level (Table 2, Fig. 1).
- Considering the SF level data, group A showed statistically significant higher values of SF than group B at baseline (group A, 95.49±21.53 ng/mL and group B, 44.86±4.69 ng/mL; p=0.018). Whereas group B showed statistically lower (group A, 77.06±14.06 ng/mL and group B, 39.05±5.46 ng/mL; p=0.009) SF level compared to group A after 3 months of NSPT (Table 3, Fig. 2). However, no significant alteration (p=0.618) in SF level was observed in group A after 3 months of treatment compared to the baseline level. However, the SF level in group B decreased significantly (p=0.039) after 3 months of NSPT compared with the corresponding baseline level (Table 3, Fig. 2).
Results
- The underlying anemia status in smokers may be masked by relatively higher Hb values, which are usually tested to assess anemia. This may lead to an underestimation of the prevalence of anemia among smokers. The available literature suggests that only a few studies have analyzed the efficacy of periodontal interventions, such as NSPT, on the anemia status of such patients by assessing SE or SF.
- In the present study, the baseline mean SE levels were significantly lower (p=0.031) in smokers with CP than in nonsmokers with CP. In addition, SE levels were negatively correlated with smoking at baseline. These findings are consistent with those of Tanabe et al. [16] and Eisenga et al. [17]. During daytime smoking, higher SE levels lead to erythrocytosis, which in turn inhibits further erythropoietin production through a negative feedback loop. Endogenous circulating erythropoietin with a half-life of 6 to 8 hours would result in low SE in the morning hours when blood samples are usually drawn [17]. This phenomenon is supported by the circadian rhythm of SE levels described by Miller et al. [18]. An alternative explanation may be derived from the study by Weinberg et al. [19] who observed the JAK2 V617F mutation in cigarette smokers and suggested that the erythrocytosis observed in smokers occurs via an erythroid cell-intrinsic erythropoietin-independent mechanism. They also stated that this may be an unidentified direct effect of smoking on erythropoiesis. Chronic smoking initially induces an increase in erythrocyte volume, plasma volume, and erythropoietin concentration, the latter of which is reduced when the erythrocyte volume increases. Hence, erythropoietin production represents a balance between stimulation by hypoxia and negative feedback by increasing erythrocyte volume [14]. The release of proinflammatory cytokines from peripheral neutrophils and various parameters of inflammation in plasma seem to be affected more by cigarette smoking than periodontal disease, which might contribute to the downregulation of erythropoietin production. Elevation of these inflammatory mediators leads to inhibition of the hormone erythropoietin and erythropoiesis, leading to the development of anemia [20].
- In the present study, 3 months following the NSPT intervention, SE levels increased from baseline values in group A, although they were not statistically significant (p=0.253). In contrast, the group B patients showed a statistically significant (p=0.035) improvement in SE levels following periodontal intervention. This is in agreement with the results of Miller et al. [21], who failed to detect differences in SE levels when the COHb concentration changed following smoking cessation. As a possible explanation, they mentioned that small changes in COHb were not sufficient to trigger an erythropoietin response in persons with normal lung function. In the present study, the mean SF levels at baseline were significantly higher (p=0.018) in group A than in group B. Ghio et al. [22] supported this finding of increased SF levels among smokers compared with those among nonsmokers. They correlated this finding with the systemic accumulation of iron after cigarette smoke exposure and concluded that cigarette smoke alters iron homeostasis both in the lung and systemically. However, that study did not include patients with CP. Contradictory findings were obtained in a study by Erdemir et al. [23], who noted similar SF levels among smokers and nonsmokers. These findings were in agreement with those of patients with ACD, who had normal to elevated SF levels. However, the possible cause of the similar SF values in both groups was not explained in that report. A cross-sectional study conducted by Prakash et al. [24] assessed the anemia status of nonsmoking patients with CP by evaluating various hematological parameters. No significant changes in SF levels were observed between the study groups. In the present study, the mean SF levels in group B were significantly lower (p=0.0397) at 3 months after NSPT than at baseline. This is in agreement with the study of Chakraborty et al. [13], who detected relatively higher SF levels in smokers with CP than in nonsmokers with CP, and these levels were restored to normal following NSPT intervention. The mean SF levels in the present study at 3 months after NSPT were reduced in group A compared to baseline; however, the difference was not statistically significant (p=0.618). The available literature does not include any comparable studies.
- One limitation of the present study is its relatively small sample size. Further studies involving larger sample sizes and other parameters may be conducted in the future if required.
- Overall, NSPT leads to a relative increase in SE levels and a relative decrease in SF levels, thereby indicating an improvement in the anemia status of both smokers and nonsmokers. However, the magnitude of the changes was less in smokers. Hematological parameters such as SF and SE might serve as effective biomarkers for assessing anemia status in nonsmokers with CP. For smokers with CP, further studies with larger sample sizes may clearly demonstrate the effect of NSPT on SE and SF levels among these individuals.
Discussion
-
Conflicts of interest
No potential conflicts of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization: all authors; Investigation: SS, KST; Resources: AKD, PCP, KST; Software: AKD, KST; Supervision, Validation: SB; Data curation: AKD, RB, KST; Formal analysis: SB, RB, PCP; Methodology: SB, RB, PP, KST; Project administration: SS, AKD, PCP, KST; Visualization: AKD, PCP; Writing - original draft: SS, AKD, PP; Writing - review & editing: SS, PCP.
Notes
| Demographic variable | Group A | Group B | p-value |
|---|---|---|---|
| No. of patients | 15 | 15 | |
| Age (yr) | 47.73±2.33 | 41.93±2.79 | 0.122a) |
| Sex, male:female | 9 (60.0):6 (40.0) | 7 (46.7):8 (53.3) | 0.457b) |
| Time |
Serum erythropoietin level (mIU/mL) |
p-valuea) | |
|---|---|---|---|
| Group A (n=15) | Group B (n=15) | ||
| Baseline | 11.84±1.24 | 15.19±0.79 | 0.031 |
| At 3 mo | 13.00±1.40 | 17.74±1.36 | 0.022 |
| p-valueb) | 0.253 | 0.035 | |
| Time |
Serum ferritin level (ng/mL) |
p-valuea) | |
|---|---|---|---|
| Group A (n=15) | Group B (n=15) | ||
| Baseline | 95.49±21.53 | 44.86±4.69 | 0.018 |
| At 3 mo | 77.06±14.06 | 39.05±5.46 | 0.009 |
| p-valueb) | 0.618 | 0.039 | |
- 1. Means RT Jr, Krantz SB. Progress in understanding the pathogenesis of the anemia of chronic disease. Blood 1992;80:1639–47.PubMed
- 2. Weiss G. Pathogenesis and treatment of anaemia of chronic disease. Blood Rev 2002;16:87–96.ArticlePubMed
- 3. Naik V, Acharya A, Deshmukh VL, Shetty S, Shirhatti R. Generalized, severe, chronic periodontitis is associated with anemia of chronic disease: a pilot study in urban, Indian males. J Investig Clin Dent 2010;1:139–43.ArticlePubMed
- 4. Mullally BH. The influence of tobacco smoking on the onset of periodontitis in young persons. Tob Induc Dis 2004;2:53–65.ArticlePubMedPMC
- 5. Aitchison R, Russell N. Smoking: a major cause of polycythaemia. J R Soc Med 1988;81:89–91.ArticlePubMedPMC
- 6. Shirmohamadi A, Chitsazi MT, Faramarzi M, Salari A, Naser Alavi F, Pashazadeh N. Effect of non-surgical periodontal treatment on transferrin serum levels in patients with chronic periodontitis. J Dent Res Dent Clin Dent Prospects 2016;10:169–75.ArticlePubMedPMC
- 7. Chow JK, Werner BG, Ruthazer R, Snydman DR. Increased serum iron levels and infectious complications after liver transplantation. Clin Infect Dis 2010;51:e16–23.ArticlePubMed
- 8. Nordenberg D, Yip R, Binkin NJ. The effect of cigarette smoking on hemoglobin levels and anemia screening. JAMA 1990;264:1556–9.ArticlePubMed
- 9. Jelkmann W. Proinflammatory cytokines lowering erythropoietin production. J Interferon Cytokine Res 1998;18:555–9.ArticlePubMed
- 10. Singh V, Tanwar AS, Hungund AS, Hungund SA, Nagaraja C. Comparison of serum erythropoietin levels in smokers and nonsmokers with periodontitis: a biochemical study. J Indian Soc Periodontol 2016;20:249–53.ArticlePubMedPMC
- 11. Hutter JW, van der Velden U, Varoufaki A, Huffels RA, Hoek FJ, Loos BG. Lower numbers of erythrocytes and lower levels of hemoglobin in periodontitis patients compared to control subjects. J Clin Periodontol 2001;28:930–6.ArticlePubMed
- 12. Morley JJ, Kushner I. Serum C-reactive protein levels in disease. Ann N Y Acad Sci 1982;389:406–18.ArticlePubMed
- 13. Chakraborty S, Tewari S, Sharma RK, Narula SC. Effect of non-surgical periodontal therapy on serum ferritin levels: an interventional study. J Periodontol 2014;85:688–96.ArticlePubMed
- 14. Caton JG, Armitage G, Berglundh T, Chapple I, Jepsen S, Kornman KS, et al. A new classification scheme for periodontal and peri-implant diseases and conditions: introduction and key changes from the 1999 classification. J Clin Periodontol 2018;45 Suppl 20:S1–8.ArticlePubMed
- 15. National Center for Health Statistics (NCHS); Centers for Disease Control and Prevention. National Health Interview Survey. Glossary terms [Internet]. Hyattsville, MD: NCHS; 2017 [cited 2017 Aug 29]. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm.
- 16. Tanabe N, Ohnishi K, Fukui H, Ohno R. Effect of smoking on the serum concentration of erythropoietin and granulocyte-colony stimulating factor. Intern Med 1997;36:680–4.ArticlePubMed
- 17. Eisenga MF, Kieneker LM, Touw DJ, Nolte IM, van der Meer P, Huls G, et al. Active smoking and hematocrit and fasting circulating erythropoietin concentrations in the general population. Mayo Clin Proc 2018;93:337–43.ArticlePubMed
- 18. Miller ME, Garcia JF, Cohen RA, Cronkite EP, Moccia G, Acevedo J. Diurnal levels of immunoreactive erythropoietin in normal subjects and subjects with chronic lung disease. Br J Haematol 1981;49:189–200.ArticlePubMed
- 19. Weinberg I, Borohovitz A, Krichevsky S, Perlman R, Ben-Yehuda A, Ben-Yehuda D. Janus Kinase V617F mutation in cigarette smokers. Am J Hematol 2012;87:5–8.ArticlePubMed
- 20. Fredriksson MI, Figueredo CM, Gustafsson A, Bergström KG, Asman BE. Effect of periodontitis and smoking on blood leukocytes and acute-phase proteins. J Periodontol 1999;70:1355–60.ArticlePubMed
- 21. Miller ME, Chandra M, Garcia JF. Clinical applications of measurement of serum immunoreactive levels of erythropoietin. Ann N Y Acad Sci 1985;459:375–81.ArticlePubMed
- 22. Ghio AJ, Hilborn ED, Stonehuerner JG, Dailey LA, Carter JD, Richards JH, et al. Particulate matter in cigarette smoke alters iron homeostasis to produce a biological effect. Am J Respir Crit Care Med 2008;178:1130–8.ArticlePubMed
- 23. Erdemir EO, Nalcaci R, Caglayan O. Evaluation of systemic markers related to anemia of chronic disease in the peripheral blood of smokers and non-smokers with chronic periodontitis. Eur J Dent 2008;2:102–9.ArticlePubMedPMC
- 24. Prakash S, Dhingra K, Priya S. Similar hematological and biochemical parameters among periodontitis and control group subjects. Eur J Dent 2012;6:287–94.ArticlePubMedPMC
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine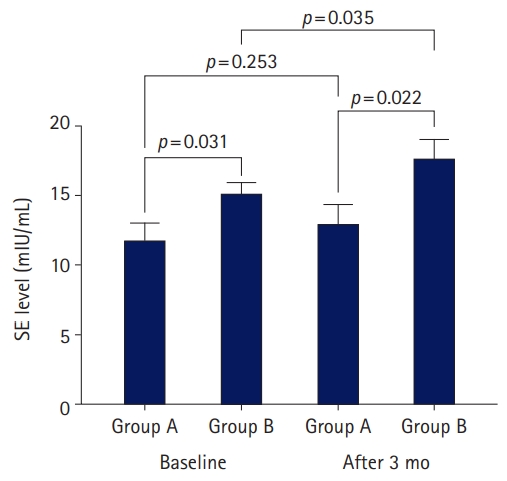

 PubReader
PubReader ePub Link
ePub Link Cite
Cite