PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(Suppl); 2023 > Article
-
Case report
Unusual presentation of asymptomatic subacute lead-related ventricular perforation beyond the pericardium without pericardial effusion: a case report -
Jihee Son1
 , Lae-Young Jung1,2,3
, Lae-Young Jung1,2,3
-
Journal of Yeungnam Medical Science 2023;40(Suppl):S105-S108.
DOI: https://doi.org/10.12701/jyms.2023.00171
Published online: May 31, 2023
1Division of Cardiology, Department of Internal Medicine, Jeonbuk National University Hospital and Jeonbuk National University Medical School, Jeonju, Korea
2Research Institute of Clinical Medicine, Jeonbuk National University, Jeonju, Korea
3Biomedical Research Institute, Jeonbuk National University Hospital, Jeonju, Korea
- Corresponding author: Lae-Young Jung, MD, PhD Division of Cardiology, Department of Internal Medicine, Jeonbuk National University Hospital and Jeonbuk National University Medical School, 20 Geonji-ro, Deokjin-gu, Jeonju 54907, Korea Tel: +82-63-250-1389 • Fax: +82-63-250-1680 • E-mail: lyjung@jbnu.ac.kr
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 705 Views
- 35 Download
Abstract
- The clinical manifestations of subacute pacemaker lead-related cardiac perforations are highly variable. Patients with subacute perforations can present with a variety of symptoms, whereas those with acute perforations usually present with cardiac tamponade that necessitates emergent pericardiocentesis. A 32-year-old woman underwent pacemaker implantation for sick sinus syndrome. An active-fixation atrial lead was fixed to the right atrial appendage, and a ventricular lead was fixed to the right ventricle (RV) apex, with acceptable parameters. Two weeks postoperative, the patient visited the clinic for routine examination of the pacemaker parameters. Chest X-ray showed migration of the RV lead beyond the cardiac silhouette. Echocardiography revealed no evidence of pericardial effusion or tamponade. Computed tomography revealed that the RV lead was positioned beyond the RV and pericardium and into the anterior chest wall. Procedural lead revision was performed with cardiothoracic surgery backup. The lead was retracted after loosening the active-fixation screw and inserting the stylet. The lead was placed in the RV septum with active fixation. The procedure was completed without complications, and the patient was discharged after 3 days. Subacute lead perforations can present with various symptoms, and some patients may be asymptomatic without pericardial effusion. Altered lead parameters frequently provide the first indication for the diagnosis of cardiac perforation. Transvenous lead revision with surgical backup is an alternative to surgical extraction.
- Pacemaker lead-related cardiac perforation is a serious complication after pacemaker implantation, with a reported incidence of 0.1% to 0.8% [1]. Clinical presentations vary widely, from asymptomatic to sudden cardiac arrest. Most cases occur early after implantation and are accompanied by pericardial effusion. Moreover, optimal management of this complication remains controversial. For the migration of a lead outside the pericardial space, current therapy entails surgical extraction and implantation of a new lead. However, several recent studies have reported percutaneous lead revision as an alternative to surgery [2]. In this report, we describe a patient with an unusual presentation of asymptomatic subacute lead-related cardiac perforation beyond the pericardium without pericardial effusion.
Introduction
- Ethical statements: This study was approved by the Institutional Review Board (IRB) of Jeonbuk National University Hospital (IRB No: CUH 2023-04-012). Informed consent was obtained from the patient.
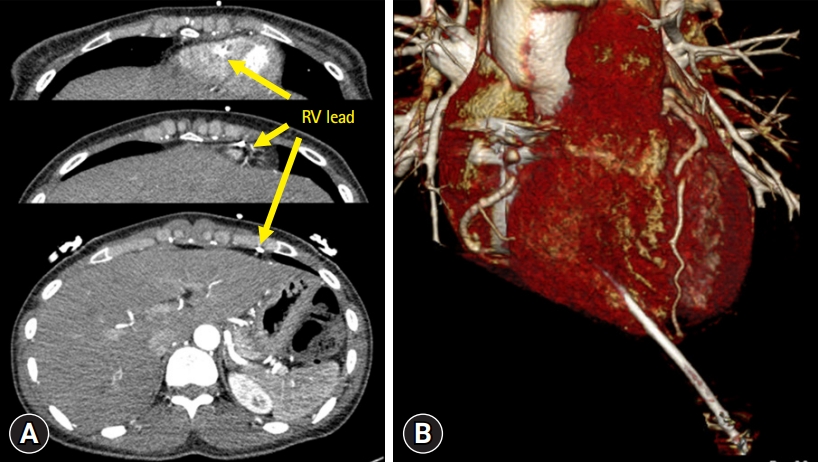
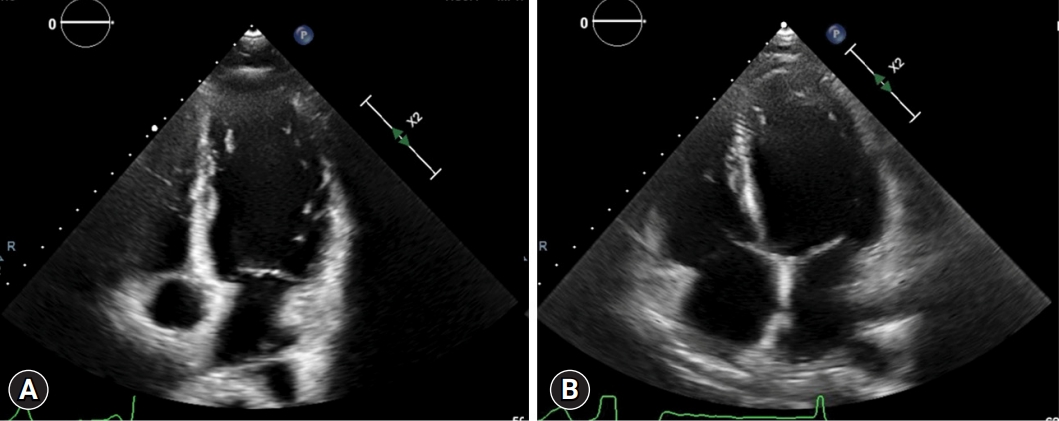
- A 32-year-old woman underwent pacemaker implantation for sick sinus syndrome. An active-fixation atrial lead (DDDR; Boston Scientific Inc., Marlborough, MA, USA) was fixed to the right atrial appendage, and a ventricular lead was fixed to the right ventricle (RV) apex, with acceptable parameters (Fig. 1A). Two weeks postoperative, the patient visited our clinic for routine pacemaker examination. Device interrogation revealed sensing and capture failures of the RV lead. Chest X-ray showed migration of the RV lead beyond the cardiac silhouette (Fig. 1B). There was no evidence of pericardial effusion or tamponade by echocardiography despite perforation of the RV lead (Fig. 2); hence, computed tomography (CT) was performed. Chest CT demonstrated that the RV lead was positioned beyond the RV and pericardium, and into the anterior chest wall (Fig. 3). Procedural lead revision was performed with cardiothoracic surgery backup. The lead was retracted after loosening the active-fixation screw and inserting the stylet. Transthoracic echocardiography revealed no pericardial effusion, and the patient’s vital signs were stable. The lead was then placed on the RV septum with active fixation (Fig. 1C). The procedure was completed without complications, and the patient was discharged after 3 days.
Case
- Cases of subacute lead perforation (those diagnosed 1–30 days after implantation) are less common than acute lead perforations [1]. Furthermore, clinical manifestations are highly diverse. Patients with subacute or delayed lead perforation can present with various clinical manifestations and many patients may remain asymptomatic, whereas those with acute lead perforation usually present with cardiac tamponade. The exact mechanism underlying subacute lead-related perforations is not fully understood. Although acute perforation can occur if the lead tip is forced through the myocardium, subacute perforation is a more gradual process, possibly due to altered durability of the myocardial wall or continuous mechanical force from the pacemaker lead [2,3]. These mechanisms explain the low prevalence of cardiac tamponade associated with subacute lead-related perforations. Issa and Issa reported that gradual changes produce self-sealing properties through muscle contraction, fibrosis, or the lead itself, which may reduce the risk of rapidly progressing pericardial effusion [2]. In a recent study, only eight of 54 patients (14.8%) with subacute and delayed lead perforations presented with pericardial effusion [3].
- Because patients with subacute perforation can be asymptomatic, lead perforation can be identified incidentally via radiographic findings, which suggest lead migration or abnormal lead parameters during routine pacemaker interrogation tests. A previous study reported that altered lead electrical parameters at device interrogation in the culprit lead, compared to immediate postimplantation parameters, were observed in almost all patients with subacute lead perforation. In that study, 42.5% of the patients were asymptomatic [3]. Therefore, altered lead parameters are often the first indications of lead perforation. A chest X-ray or CT scan can be helpful when a patient presents with cardiac perforation during a routine check-up.
- The optimal management of subacute lead perforations remains debatable. Recently, several reports proposed transvenous procedural lead revision with surgical backup as an alternative to surgical extraction. The complete procedural success rates reported in these studies were as high as 90% [4]. In a previous study, no cardiac tamponade was reported during or after the procedure [2]. Low pressure in the RV, myocardial “self-sealing” properties, and fibrotic changes at the perforating lesion are supportive of recovery of the perforated myocardium [4].
- Our case demonstrates the potential for subacute pacemaker lead-related RV perforation after successful pacemaker implantation. The pacing lead migrated through the RV wall and the patient remained asymptomatic without pericardial effusion, which are unusual features of this complication. In the absence of bleeding from the pierced RV, the lead was intravenously repositioned. Repositioning acts as curative management and can be performed without further complications.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization, Investigation, Resources: LYJ; Writing-original draft: JS, LYJ; Writing-review & editing: LYJ.
Notes


- 1. Vamos M, Erath JW, Benz AP, Bari Z, Duray GZ, Hohnloser SH. Incidence of cardiac perforation with conventional and with leadless pacemaker systems: a systematic review and meta-analysis. J Cardiovasc Electrophysiol 2017;28:336–46.ArticlePubMedPDF
- 2. Issa ZF, Issa TZ. Feasibility and safety of percutaneous lead revision for subacute and delayed cardiac device lead perforation. JACC Clin Electrophysiol 2021;7:26–35.ArticlePubMed
- 3. Archontakis S, Sideris K, Aggeli K, Gatzoulis K, Demosthenous M, Tolios P, et al. Percutaneous lead extraction and repositioning: an effective and safe therapeutic strategy for early ventricular lead perforation with dislocation both inside and outside the pericardial sac following a cardiac device implantation. J Cardiovasc Electrophysiol 2019;30:299–307.ArticlePubMedPDF
- 4. Zhou X, Ze F, Li D, Wang L, Guo J, Li X. Outcomes of transvenous lead extraction in patients with lead perforation: a single-center experience. Clin Cardiol 2020;43:386–93.ArticlePubMedPMCPDF
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite