PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(4); 2023 > Article
-
Case report
Endovascular treatment of Takayasu arteritis in a middle-aged woman with syncope and limb claudication: a case report -
Ha-Young Choi1
 , Sunggun Lee2
, Sunggun Lee2 , Jino Park1
, Jino Park1 , Yeo-Jeong Song1
, Yeo-Jeong Song1 , Dong-Kie Kim1
, Dong-Kie Kim1 , Ki-Hun Kim1
, Ki-Hun Kim1 , Sang-Hoon Seol1
, Sang-Hoon Seol1 , Doo-Il Kim1
, Doo-Il Kim1 , Seunghwan Kim1
, Seunghwan Kim1
-
Journal of Yeungnam Medical Science 2023;40(4):448-453.
DOI: https://doi.org/10.12701/jyms.2023.00122
Published online: April 26, 2023
1Division of Cardiology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
2Division of Rheumatology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- Corresponding author: Seunghwan Kim, MD Division of Cardiology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, 875 Haeun-daero, Haeundae-gu, Busan 48108, Korea Tel: +82-51-797-3070 • Fax: +82-51-797-3009 • E-mail: cloudksh@gmail.com
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 901 Views
- 37 Download
Abstract
- Takayasu arteritis (TA) is a disease that causes inflammation and stenosis of medium to large blood vessels. We report a case of a 50-year-old female patient with newly developed hypertension, syncope, and claudication of the extremities. Total occlusion of the left subclavian artery at the origin was found and significant stenosis of the right common iliac artery was revealed by hemodynamic analysis. She was successfully treated with percutaneous angioplasty for multiple peripheral arterial diseases and was finally diagnosed with TA. In consultation with a rheumatologist, medical treatment for TA was initiated, the patient’s hypertension disappeared, and her claudication symptoms improved.
- Takayasu arteritis (TA) is a rare vascular inflammatory disease that is common in young Asian women, mainly between the ages of 10 to 40 years [1]. TA is divided into five types according to the arteries involved, and its clinical manifestations vary depending on the affected blood vessels [2]. TA is divided into types I, IIa, and IIb depending on whether the ascending or descending aorta is involved with the invasion of the aortic arch and branches. Types III, IV, and V are determined according to the association of the abdominal aorta and combined features.
- Herein, we report a case of a middle-aged female patient who complained of syncope and claudication due to multiple peripheral arterial stenoses caused by not typical atherosclerosis but TA, which was successfully treated with a combination of endovascular and immunosuppressive therapies.
Introduction
- Ethical statements: This study was exempted from review by the Institutional Review Board (IRB) of Inje University Haeundae Paik Hospital (IRB No: 2022-10-003), and the requirement for informed consent from the patient was waived by the IRB.
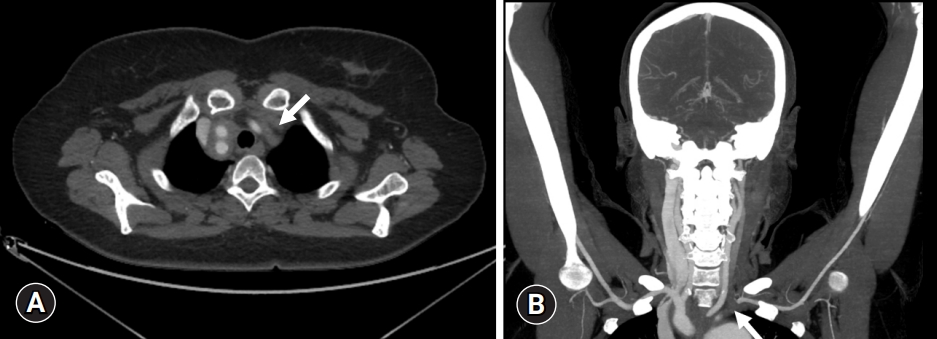
- A 50-year-old female patient with a history of recently diagnosed hypertension presented with syncope that occurred when she was replacing a fluorescent lamp. Further, history taking revealed that she started experiencing claudication in her left arm and right thigh 6 months earlier. On physical examination, blood pressure in the right and left arms was 180/40 and 80/40 mmHg, respectively. Because of this unusual blood pressure differential, computed tomography angiography (CTA) of the upper extremity was performed, which showed total occlusion of the left subclavian artery at the origin (Fig. 1). Since the patient had no neurological signs or abnormal findings on brain computed tomography (CT) scan, it was inferred that the syncope occurred due to subclavian steal syndrome due to total occlusion of the left subclavian artery [3].
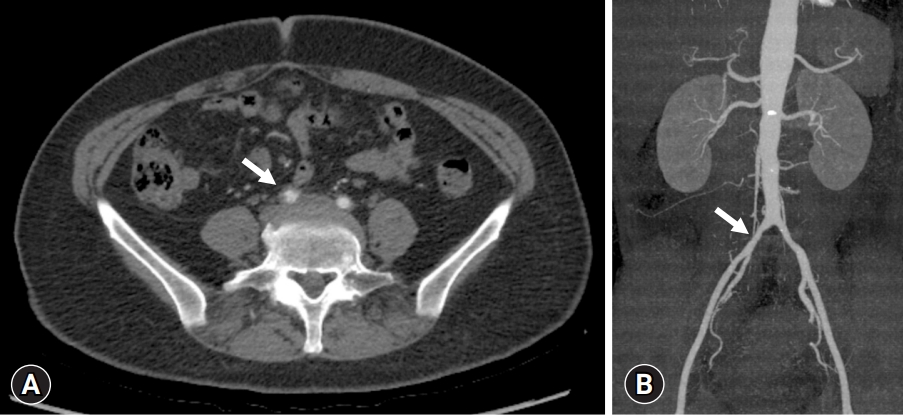
- To evaluate the patient’s right thigh pain when walking uphill, an ankle-brachial index (ABI) test and lower extremity CTA were performed. The ABI was lower for the right leg than for the left leg (0.81 and 0.94, respectively), although the lower extremity CTA showed approximately 30% focal mild stenosis of both common iliac arteries (CIAs) (Fig. 2).
- Two options are available for the treatment of left subclavian artery occlusion: bypass surgery and percutaneous transluminal angioplasty (PTA). However, we chose PTA among the two options because we wanted to evaluate the reason for right claudication with discordant results between the lower extremity CTA and ABI test. We also considered that PTA of the total occlusion of the left subclavian artery was a less invasive procedure to preserve blood flow to the brain resulting from subclavian steal syndrome [4].
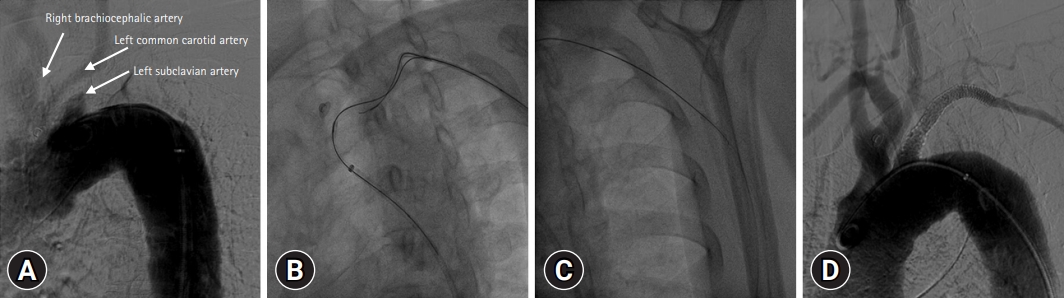
- The right common femoral artery was punctured, and both iliac angiographies using pigtail catheter were performed. Angiography revealed a flap-like lesion with mild stenosis in the right CIA (Fig. 3A). We conducted a hemodynamic analysis because the mild lesion shown on CTA did not match the patient’s symptoms and low ABI. The catheter-guided translesional pressure gradient of the right CIA was 60 mmHg (Fig. 3B, 3C), which was judged to be hemodynamically significant vascular stenosis [5]. Therefore, we decided to perform an intervention for the stenotic lesion of the right CIA after PTA of the left subclavian artery.
- For the left subclavian artery lesion, angiography revealed diffuse total occlusion of the left subclavian artery (Fig. 4A). Since the passage of the antegrade guidewire was blocked by a hard proximal lesion, the left radial artery was punctured for bidirectional guidewire placement. After negotiating the bidirectional guidewires, we advanced the antegrade guidewire in the right direction through the intraluminal space (Fig. 4B) and positioned the retrograde guide sheath (Fig. 4C). After successful passage of the guidewire through the lesion, stepwise balloon angioplasty was performed using a 2.5×100-mm Sterling SL small balloon (Boston Scientific, Natick, MA, USA) and 6.0×40-mm Armada 35 (Abbott Vascular, Redwood, CA, USA). Predilatation with the 6.0×40-mm Armada 35 could not be performed because of the hard total occluded lesion. Follow-up angiography revealed >70% residual stenosis with a large difference in landing zone diameter between the proximal and distal ends. Therefore, a balloon expandable stent (7.0×59-mm Omnilink, Abbott Vascular) was inserted, and postdilatation using a 9.0×40-mm POWERFLEX PRO (Cordis, Miami, FL, USA) was performed. Final angiography revealed no residual stenosis, with good flow in the left subclavian artery (Fig. 4D).
- For the right CIA lesion, the guidewire was passed through the lesion, and balloon angioplasty was performed several times with a 7.0×40-mm Armada 35 catheter. Follow-up angiography revealed >30% residual stenosis with a small dissection. Therefore, a self-expandable stent (8.0×40-mm Absolute Pro, Abbott Vascular) was inserted, and postdilatation was performed using a 7.0×40-mm Armada 35 catheter. Final angiography revealed no residual stenosis with good flow (Fig. 5). One day after the procedure, a follow-up ABI test was performed, showing improved values (1.21 for the right and 1.28 for the left).
- In this patient, CTA showed localized wall thickening in the right brachiocephalic and right subclavian arteries, total occlusion of the left subclavian artery at the origin, and focal stenosis of both CIAs, without typical atherosclerotic arterial disease. Additionally, the patient had no risk factors for atherosclerosis, except for newly developed hypertension. Typical CT findings of TA include concentric mural thickening and luminal stenosis in the aorta and its main branches [6]. Based on the above findings and diagnostic criteria [7], TA was diagnosed and classified as type IIa according to the angiographic classification [2].
- The patient’s C-reactive protein level was elevated at 1.20 mg/dL and the erythrocyte sedimentation rate was 43 mm at the time of first admission, which was considered an active stage of the disease [8]. In cooperation with a rheumatologist, standard medical treatment for A, including methylprednisolone (MPD) and methotrexate was initiated. Because weight-adapted steroid dosages have not been strictly tested in clinical trials, the present recommendations only suggest dose ranges [8]. The initial dose of MPD was administered intravenously at 40 mg, followed by the same oral maintenance dose for 1 week. At an outpatient clinic, the MPD was tapered to 32 mg, 16 mg, and 12 mg at 2-week intervals, followed by 6 mg for 1 week, 4 mg for 4 weeks, and 2 mg for 8 weeks, after which MPD treatment was stopped. Methotrexate was started at 7.5 mg and has been maintained to date. The patient showed an improvement in symptoms and was discharged from the hospital. Subsequently, her hypertension disappeared without antihypertensive medications during outpatient follow-up, and her symptoms improved.
Case
- TA is a vasculitis involving large and medium-sized vessels, and the initial obligatory diagnosis criterion for TA is age under 40 years [1]. However, there have been many studies and cases in middle-aged individuals who are older than 40 years of age. Accordingly, age was deleted from the diagnostic criteria to produce the modified diagnostic criteria for TA [9]. Although the diagnostic criteria have changed, there is still a preconception that TA occurs mainly at a young age. Therefore, we did not initially suspect that this patient had TA because she was in her 50s.
- The patient visited our hospital with syncope as the chief complaint, and the neurological signs and radiologic images showed that the cause of the symptom was subclavian steal syndrome rather than a brain abnormality. Subclavian steal syndrome is a temporary phenomenon of vertebrobasilar ischemia caused by occlusion or stenosis of the proximal subclavian artery, which “steals” blood flow from the contralateral vertebral artery, creating retrograde flow in the ipsilateral vertebral artery [3,10]. Syncope may occur due to this transient cerebral ischemia.
- In this case, the TA invaded the branches of the ascending aorta and was classified as type IIa by angiographic classification. According to the study by Hata et al. in 1996 [2], which analyzed the angiographic findings of TA patients, type IIa accounted for approximately 11% of the total TA patients in that study. This was not a high prevalence in the TA patient group, but the number was not small. Therefore, we hope that our case report will provide details about the treatment of this patient group and help future patients.
- The arterioplastic approach is considered in TA patients with symptoms of arterial stenosis such as limb claudication, ischemic episodes, uncontrolled renovascular hypertension, or angina [11]. Although there are concerns about restenosis after PTA, a retrospective study on stenting of 177 subclavian or innominate arteries from 1993 to 2006 showed encouraging results that primary patency (defined as uninterrupted vascular patency without repeat intervention) was 84% at 5 years and secondary patency (defined as maintenance of patency requiring a repeat intervention) was 98% at 4 years [12]. PTA also resulted in low procedural stroke and death rates (0.6%). As endovascular treatment has gradually developed, percutaneous revascularization with stenting has been preferred over surgical treatment as first-line therapy in recent years [12-15].
- The reason why we chose PTA in this case was not only to preserve blood flow to the brain with fewer major complications in subclavian steal syndrome [16-18] but also to evaluate via functional assessment the exact vascular state of the right CIA due to reduced ABI and claudication symptoms. Because the results of peripheral angiography and hemodynamic assessment confirmed total occlusion of the left subclavian artery and significant stenosis of the right common iliac artery, we selected a less invasive and effective PTA considering postoperative complications and disease stage. By combining antegrade (right femoral artery) and retrograde (left radial artery) approaches, the total occlusion of the left subclavian artery was successfully revascularized after stent insertion. The claudication symptoms of the right leg improved after endovascular treatment of the right CIA, and the follow-up ABI returned to within normal limits.
- The significance of this case report is that a middle-aged woman presenting with syncope and claudication of the extremities was finally diagnosed with TA, which was not a typical atherosclerotic peripheral arterial disease and was successfully treated with a combination of endovascular treatment and immunosuppressive therapy, and improved multiple clinical manifestations including hypertension.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization: all authors; Investigation, Data curation: HYC; Formal analysis, Supervision: SL, JP, YJS, DKK, KHK, SHS, DIK, SK; Writing-original draft: HYC; Writing-review & editing: all authors.
Notes


- 1. Ishikawa K. Diagnostic approach and proposed criteria for the clinical diagnosis of Takayasu’s arteriopathy. J Am Coll Cardiol 1988;12:964–72.ArticlePubMed
- 2. Hata A, Noda M, Moriwaki R, Numano F. Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol 1996;54(Suppl):S155–63.ArticlePubMed
- 3. Osiro S, Zurada A, Gielecki J, Shoja MM, Tubbs RS, Loukas M. A review of subclavian steal syndrome with clinical correlation. Med Sci Monit 2012;18:RA57–63.ArticlePubMedPMC
- 4. Gu YQ, Wang ZG. Surgical treatment of cerebral ischaemia caused by cervical arterial lesions due to Takayasu’s arteritis: preliminary results of 49 cases. ANZ J Surg 2001;71:89–92.ArticlePubMedPDF
- 5. de Boer SW, Heinen S, van den Heuvel D, van de Vosse FN, de Vries J; study contributors. How to define the hemodynamic significance of an equivocal iliofemoral artery stenosis: review of literature and outcomes of an international questionnaire. Vascular 2017;25:598–608.ArticlePubMedPDF
- 6. Zhu FP, Luo S, Wang ZJ, Jin ZY, Zhang LJ, Lu GM. Takayasu arteritis: imaging spectrum at multidetector CT angiography. Br J Radiol 2012;85:e1282–92.ArticlePubMedPMC
- 7. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 1990;33:1129–34.ArticlePubMed
- 8. Hellmich B, Agueda A, Monti S, Buttgereit F, de Boysson H, Brouwer E, et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 2020;79:19–30.ArticlePubMed
- 9. Sharma BK, Jain S, Suri S, Numano F. Diagnostic criteria for Takayasu arteritis. Int J Cardiol 1996;54(Suppl):S141–7.ArticlePubMed
- 10. Yoneda S, Nukada T, Tada K, Imaizumi M, Takano T. Subclavian steal in Takayasu’s arteritis: a hemodynamic study by means of ultrasonic Doppler flowmetry. Stroke 1977;8:264–8.ArticlePubMed
- 11. Águeda AF, Monti S, Luqmani RA, Buttgereit F, Cid M, Dasgupta B, et al. Management of Takayasu arteritis: a systematic literature review informing the 2018 update of the EULAR recommendation for the management of large vessel vasculitis. RMD Open 2019;5:e001020.ArticlePubMedPMC
- 12. Patel SN, White CJ, Collins TJ, Daniel GA, Jenkins JS, Reilly JP, et al. Catheter-based treatment of the subclavian and innominate arteries. Catheter Cardiovasc Interv 2008;71:963–8.ArticlePubMed
- 13. Ogino H, Matsuda H, Minatoya K, Sasaki H, Tanaka H, Matsumura Y, et al. Overview of late outcome of medical and surgical treatment for Takayasu arteritis. Circulation 2008;118:2738–47.ArticlePubMed
- 14. Choi YK, Jung YO, Kim HM, Kang MK. A case of a patient with Takayasu arteritis treated with left subclavian artery stent implantation. J Cardiol Cases 2015;12:123–5.ArticlePubMedPMC
- 15. Satti SR, Golwala SN, Vance AZ, Tuerff SN. Subclavian steal: Endovascular treatment of total occlusions of the subclavian artery using a retrograde transradial subintimal approach. Interv Neuroradiol 2016;22:340–8.ArticlePubMedPMCPDF
- 16. Hadjipetrou P, Cox S, Piemonte T, Eisenhauer A. Percutaneous revascularization of atherosclerotic obstruction of aortic arch vessels. J Am Coll Cardiol 1999;33:1238–45.ArticlePubMed
- 17. Kandarpa K, Becker GJ, Hunink MG, McNamara TO, Rundback JH, Trost DW, et al. Transcatheter interventions for the treatment of peripheral atherosclerotic lesions: part I. J Vasc Interv Radiol 2001;12:683–95.ArticlePubMed
- 18. Brountzos EN, Malagari K, Kelekis DA. Endovascular treatment of occlusive lesions of the subclavian and innominate arteries. Cardiovasc Intervent Radiol 2006;29:503–10.ArticlePubMedPDF
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite






